Shoulder Injection Techniques
Lennard Funk & Catherine Sulzmann, 2011
Shoulder injections are used for diagnostic, as well as therapeutic purposes. The common substances injected include corticosteroids and hyaluronans.
Corticosteroids are strong anti-inflammatory medications reducing swelling and inflammation. These are often used in conjunction with physiotherapy rehabilitation and other medications for a more lasting cure of many conditions, such as subacromial impingement syndrome, AC joint pathology and inflammatory arthritides.
Hyaluronans also have anti-inflammatory benefits, as well as coating pain receptors, stimulating endogenous synovial fluid production and lubrication effects. They seem to have a role in degenerative synovial joint disease where surgery is not indicated.
Injections are often performed 'blind' (without image guidance) in the clinical setting. The more trained and skilled the clinician is, the more reliable and accurate the injection. Image guided injections are more accurate, but also require a skilled clinician who is familiar with the technique and equipment. The guide below is based on our current practice and the practice of many UK shoulder surgeons. Click here for an article on Ultrasound guided injections and here for our Ultrasound booklet which includes guided techniques.
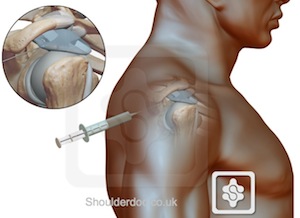
Glenohumeral joint injection
Used for pain relief of shoulder arthritis and frozen shoulder affecting the shoulder.Procedure
Posterior Approach: The patient sits with their arm resting at their side with the shoulder in neutral rotation resting on their lap. The sulcus between the head of the humerus and acromion is identified. The needle is inserted 2-3cm inferior and medial to the posterolateral corner of the acromion and directed anteriorly towards the coracoid process. An 18 gauge needle should sink completely into the joint and the plunger should push with great ease and no resistance if you are in the glenohumeral joint.
Anterior Approach: The needle is inserted medial to the head of humerus, lateral to the coracoid process by 1cm and directed posteriorly at a slight superior and lateral angle. Again, an 18 gauge needle should slip into the joint completely and the injection have no resistance.
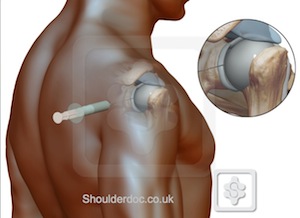
Subacromial Space injection
Used for pain relief of subacromial impingement / bursitis (subdeltoid bursitis), rotator cuff impingement or tendinosisProcedure
The patient sits with their arm resting by their side, as above. The posterior edge of the acromion is recognised, then the needle is inserted inferior to the posterolateral acromion and directed laterally into the subacromial space, aiming for the anterolateral corner of the acromion. A long 18 gauge needle should 2-3cm anterior to the posterolateral corner of the acromion and the syringe plunger should push easily with no resistance during injection. If any resistance is encountered, the needle should be with drawn and readjusted aiming more superiorly under the acromion, as the common error is to inject into the rotator cuff. This should be avoided due to the proteolytic nature of corticosteroids.
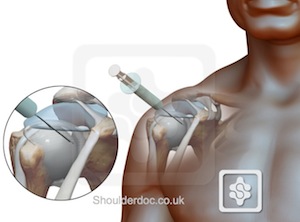
Acromioclavicular joint injection
Used for pain relief of osteolysis of the distal clavicle and osteoarthritis of the joint.Procedure
The patient sits with their arm resting at their side. The distal aspect of the clavicle is palpated to identify the convexity of the AC joint where the clavicle meets the acromion, then the needle is inserted from an anterior and superior angle and directed inferiorly. Over half of the population have an angled AC joint, so a medial direction of the needle will ensure this angle is accounted for. Again, the needle should pass easily into the joint and 2ml injected. The joint will not accommodate more than 2ml.

Long Head of Biceps (LHB) injection
Used for pain relief of biceps tendonitis where the long head of biceps is inflamedProcedure
This should be preformed under ultrasound guidance, as the biceps tendon is deep under the thick deltoid and impossible to 'feel' with the needle. Injecting the biceps tendon with a proteolytic steroid can also increase the risk of tendon rupture. Therefore, we prefer to use a hyaluronan (Ostenil) in young patients.
The patient sits with their arm resting by their side. Due to the great variation in humeral version, the tendon position can only be judged by rotating the arm into the best position for injection and letting the patient rest it their. The LHB tendon and groove are identified and marked on the skin with a marker. The point of injection, just lateral to the ultrasound probe is marked. The needle is directed at a 45 degree angle in the long axis of the probe, heading towards the LHB sheath and tendon. The actual tendon is not injected but rather the swollen sheath around the tendon. The injected fluid can be seen to run into the sheath.
Video of an ultrasound guided injection of Ostenil hyaluronan:


