Sternoclavicular Joint Injuries
Charlie Talbot, Ian Trail & Lennard Funk
- Injuries to the sternoclavicular joint (SCJ) are relatively uncommon, accounting for less than 5% of shoulder girdle injuries.
- The SCJ is generally a very stable joint due to it's very strong supporting ligaments. However, it can dislocate or become unstable.
- This may follow trauma or injury. People who have lax joint ligaments (commonly known as "double-jointed") are more prone to dislocate the SCJ.
- Following an injury the joint may become unstable and keep popping out (unstable) or remain dislocated (locked dislocation)
Sternoclavicular joint injuries are graded into three categories.
- First degree injury: a simple sprain, which involves an incomplete tear or stretching of the sternoclavicular and costoclavicular ligaments. This is the most common type of sternoclavicular joint injury.
- Second degree injury: the clavicle subluxes either anteriorly or posteriorly from its manubrial attachment, causing a complete breach of the sternoclavicular ligament but at most, only a partial tear of the costoclavicular ligament
- Third degree injury: a complete rupture of the sternoclavicular and costoclavicular ligaments, permitting a complete dislocation of the clavicle from the manubrium.
- Anterior dislocations are much more common (by a 9:1 ratio) usually resulting from an indirect action, such as a blow to the anterior shoulder that rotates the shoulder backwards thereby transmitting the stress to the sternoclavicular joint.
- Posterior dislocations are usually a result of a force driving the shoulder forwards, or from a direct impact to the superior sternal or medial clavicular surfaces. An example of the latter would be falling on a rugby ball with your team mates landing on top of you!
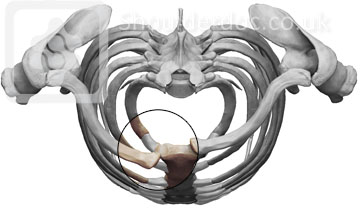
ANTERIOR DISLOCATION (viewed from above)
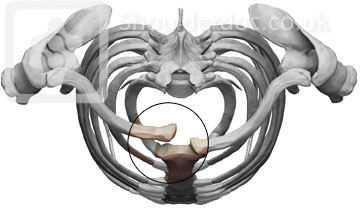
POSTERIOR DISLOCATION (viewed from above)
Treatment:
- Initial management is to try put the joint back into place. This generally requires admission to hospital and an anaesthetic.
- Most patients settle over a few weeks, but a small minority can remain unstable and painful.
- In these people the joint can be surgically stabilised.
- Surgery:
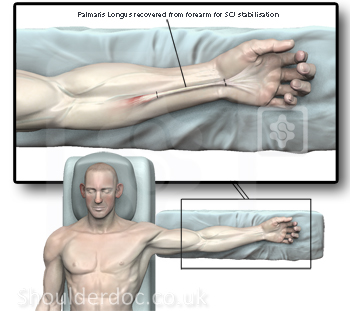
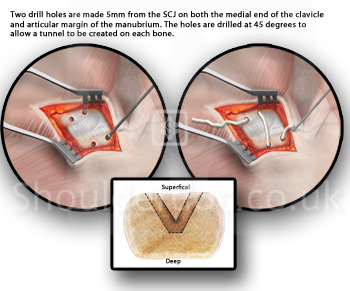
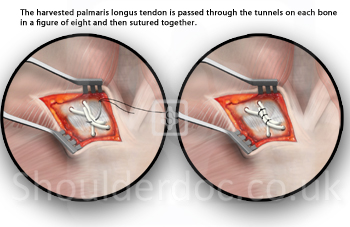
- There are a number of techniques described to stabilise the SCJ and we perform stabilisation of the joint using a free tendon graft from the forearm.
- Our technique differs by using an all anterior approach to minimise the risk to structures that lie behind the SCJ.
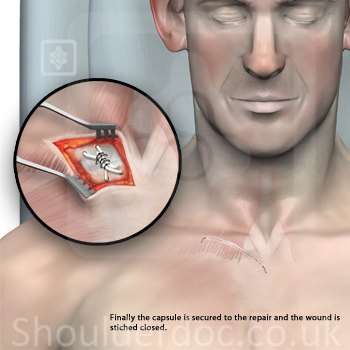
- A small skin incision is placed over the joint and the joint is reduced (held) in its anatomical position.
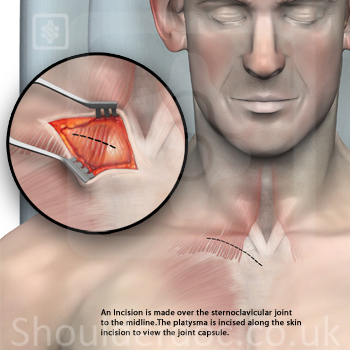
- In order to prevent repeat dislocation the tendon graft is tunnelled through the bone at the end of the collar bone, then taken across the joint and again tunnelled through the breast bone, providing a buttress at the front of the joint.
- A sling is required for six weeks.
- Physiotherapy to maintain shoulder movements are started when comfort allows and follows a graduated physiotherapy programme with supervised passive assisted range of motion exercises progressing to full active movements.


