Biceps Tenodesis
This procedure is indicated for the treatment for partial or full-thickness biceps tendon tears, severe biceps tendonopathy, or biceps instability associated with a rotator cuff tears. Biceps tenodesis involves detaching the LHB from it's superior labrum in the shoulder and reattached to the humerus bone just below the shoulder. This procedure is more complex than a tenotomy , but avoids the risks of biceps discomfort, weakness and a 'popeye' appearance.
Tenodesis is preferable for more active people. Using modern fixation screws the repair is strong enough to move the arm early after surgery.
There are two surgical techniques for this surgery. Either a mini open or a sub pectoral biceps tenodesis.
The procedure for a biceps tenodesis:
1. A beach chair or lateral position can be used.
2. The arthroscope is place in the posterior portal and a needle is passed from anterior through the biceps tendon. A suture is then passed through the needle, captured with a grabber from the anterior portal and then extracted. This is to ensure the tendon does not drop down the arm when it is cut.
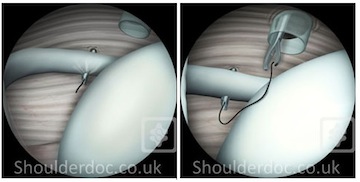
3. After the tendon is marked with a suture, an arthroscopic scissor is then used to cut the tendon from its origin.
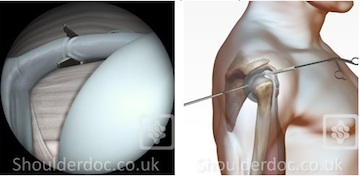
Arthroscopic scissors inserted via small puncture hole in skin and cutting the LHB (arthroscopic view on the left)
4. A small incision (2-3cm) is made over the front of the shoulder to reveal the biceps tendon:
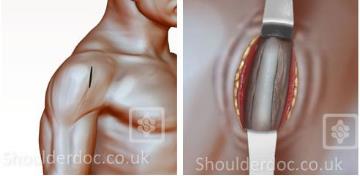
5. The biceps sheath surrounding the biceps is opened and the tendon is then delivered out of the wound
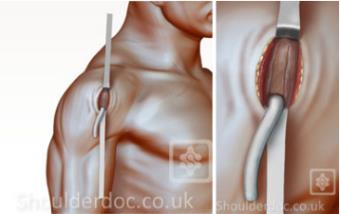
6. The tendon is trimmed and a non-absorable suture is place in the top of the tendon. A guide wire and reamer is then used to make a deep bone tunnel in the humerus.

7. The tendon is fixed back into the bone of the humerus with a special interference screw:


Video of the procedure:
GENERAL ADVICE
You should not eat or drink anything after midnight the night before the procedure.
You will usually be in hospital for no more than one day. Most people will be able to go home the same day (daycase)
Your surgeon and a physiotherapist will see you prior to discharge and you will be taught exercises to do and given further advice to guide you through your recovery.
For more information click here.
Your arm will remain in a shoulder sling for about least 3 weeks. You mainly wear the sling when out and about and for sleeping, but can remove it for dressing, bathing and light activities as guided by your physiotherapist. It does mean that you will be unable to use the arm throughout this time for most other activities. For more details onLiving with a Shoulder Sling Click Here
An appointment will be made for you to see the surgeon or specialist therapist 3 weeks post-operatively.
The length of time that you will be off work will depend on your job but expect a minimum of 3 weeks for minor tears, increasing to possibly 6 months if work involves heavy duties.
Physiotherapy will be organised for when you leave hospital and may well continue for some months after the surgery.
You will be guided through the rehabilitation programme by your physiotherapist. It is of the utmost importance that you stick strictly to this programme.
Click here for a post-op rehabilitation protocol
For more information see:
- Arthroscopic tenotomy of the long head of the biceps in the treatment of rotator cuff tears: Clinical and radiographic results of 307 cases
- The cosmetic appearance of the biceps muscle after long-head tenotomy versus tenodesis.
- Arthroscopic Release of the Long Head of the Biceps Tendon
- Long head biceps tenotomy versus tenodesis: A cadaveric biomechanical analysis
- FUNCTIONAL SYMPTOMATOLOGY FOLLOWING BICEPS TENODESIS COMPARED TO BICEPS TENOTOMY OR RUPTURE


