Operative treatment of shoulder lesions
CHAPTER VIII
WE cannot take the space in this book to describe the standard operations of amputation, excision, and arthrodesis of the shoulder joint, but we may offer the following brief suggestions for slight modifications of the usual methods.
In doing an amputation at the shoulder joint, if the pathology permits, the deltoid should be mobilized at the tubercle, pushed up as a unit preserving its axillary arterial and nerve supply, until the bursa is opened from below. The short rotators can then be divided and the head of the bone lifted off the axillary nerve. When the main vessels are tied and the rest of the arm removed, the intact deltoid can be sutured to the latissimus, teres major and pectoralis in such a way that much of the contour of the shoulder is preserved, since the nerve supply of the deltoid is not injured.
In the writer's opinion two of these operations can best be accomplished by a preliminary incision of the bursa. It is not difficult to do an excision through a bursal incision two inches long. Arthrodesis can also be done through this incision, although it is probably surer to result quickly by using a "sabre-cut" incision after the manner described by A. Bruce Gill (Journ. of Bone and Joint Surgery, Apr., 1931, Vol. XIII, No. 2, p. 287).
Operations on the shoulder joint may be done for the following pathologic conditions:
Tuberculosis of the head of the humerus.
Complicated fractures and dislocations.
Infantile dislocations.
Habitual dislocations.
Deformities due to paralyses.
Tumors of adjacent bones.
Tendinitis with or without calcified deposits.
Complete rupture of the supraspinatus tendon.
Rupture of the long head of the biceps tendon.
Adhesions, bands and villi in the subacromial bursa.
We must confine this chapter to the three chief operations which the writer is in a great measure responsible for suggesting to the profession. These are: first, the technique for the removal of calcified deposits; second, the suture of complete ruptures of the supraspinatus ; and third, the "sabre-cut" incision for major operations about the shoulder joint.
THE TECHNIQUE OF THE OPERATION FOR REMOVAL OF CALCIFIED DEPOSITS
In most cases this operation can be done through an incision about one-half inch in length, but it will be perhaps safer for both patient and surgeon if an incision an inch and one-half is made to allow ample room to identify the anatomic landmarks. I will assume that the incision is of this size, although I have developed a technique of doing it through an incision just large enough to admit a nasal speculum with recurved tips. The only objects of this modification are to have less scar and less chance of intrabursal adhesions and perhaps less postoperative pain. Since even with the larger wound, i.e., one inch and one-half, opening the bursa as widely as possible, the scar is small and postoperative pain slight, and adhesions more of theoretic than practical importance, one should not hesitate at any time to enlarge a half-inch wound.
.jpg)
FIGURE 49
On the left is a figure showing the size of the open exploratory incision, which is also sufficiently large for the removal of most calcined deposits. The figure on the right shows the size to which it is necessary to enlarge the incision in order to suture a rupture of the supraspinatus by the author's method. Both figures depict a normal bursa with the edges of the roof caught with sutures and held apart to show the smooth, white, convex base which covers the tuberosity and insertions of the tendons. In the lower portion of both figures a nictitating fold is represented. By rotation of the humerus, the whole base of the bursa may be inspected through the small left-hand incision. Lesions are seldom found at any other situation than on that part of this base which is just above the greater tuberosity. The writer believes that the little exploratory incision is almost harmless, provided the surgeon understands what he is looking for and does not attempt to explore further if the pathology is not at once evident when the bursa is opened.
Anaesthesia.
I prefer to do this operation under local anaesthesia in suitable cases, because it is easier for the patient. However, it is easier for the surgeon to have the patient under general anaesthesia, because local anaesthesia does not relax the spasm, and renders it necessary to be more accurate in cutting down directly on the lesion. Even if no spasm is present before making the incision, it may be started up by touching the inflamed region with a retractor or other instrument. In a recent case the reflex spasm could be produced at will by touching the surface near the lesion, yet the touch of the instrument caused no sensation of pain. The patient was an intelligent doctor, and could describe his sensations accurately. When the retractors were out of the wound he could rotate the arm, but when they were in the wound he found himself unable to overcome the spasm by force of will, although he felt no pain except when I endeavored to force the rotation.
Although the operation can be done under such circumstances, it is unsatisfactory. I have found it so difficult to anaesthetize the base of the bursa where the deposit is, that now I do not attempt to do so. The tendon near its insertion is so dense that it is difficult to inject the novocaine, and this is as painful as incising the tendon; possibly more so.
Local anaesthesia does not permit a thorough exploration of the bursa, but when one is familiar with the local anatomy one does not need to see the whole bursa. When the patient is under ether, by a certain maneuver the arm can be pulled downward and forward, and the surgeon's forefinger introduced between the tuberosities and the acromion. When air once gets into this opening the atmospheric pressure is overcome, and the subacromial space remains open, permitting inspection and palpation of the whole bursa. This maneuver is more especially useful in cases of rupture of the tendon. In this case the joint is not held together either by atmospheric pressure or by the tension of muscles. Manipulation of this type is not necessary, and cannot, of course, often be done under local anaesthesia, but probably might be done under regional anaesthesia. I regard the latter as too serious a procedure, and would prefer a general anaesthetic.
From the patient's point of view, in spite of these drawbacks I favor a local anaesthetic, provided the surgeon knows where the deposit is, and can go directly to it through a small incision. It is then a trivial operation. But if the deposit cannot be accurately localized, and the anatomy is not clear in the surgeon's mind, general anaesthesia would be preferable in order to allow for some unnecessary manipulation and rough handling. I have operated on many doctors, and had a chance to hear their commendations or objections. I am told that the actual curetting of the lesion is painful, but not more than can be readily borne. The incision of the skin and muscle, and of the bursal roof, is not felt at all.
Some patients are obviously poor subjects for local, and others for general anaesthesia. Surgical judgment on general principles is needed. I should advise any surgeon to do his first few cases under ether, for in spite of all the directions I can give, the anatomy is difficult to describe, and one is easily confused unless very familiar with it. The facts that the structures to the right or left of this small wound are reversed in relation to the surgeon's position as to whether he stands on the acromial or axillary side of the wound, and are also reversed in right and left shoulders, add to the puzzle.
.jpg)
FIGURE 50. OPERATIVE POSITION
This is an important figure. The writer did not realize the advantage of placing the patient in this position, until he had done many of these operations, which had been attempted with the patient either in recumbency or in a sitting posture, strapped in a chair. The latter was a very satisfactory position after the strapping had been adjusted if the assistants could be trained to work in this unusual attitude. However, the cases were too infrequent for any routine to be established. Until one operates on these cases one does not realize how elusive is the shoulder on the operating table, and, since the field is entirely controlled by the position of the humerus in relation to the scapula, how any minute change in the position of either the arm or of the body is at once transmitted to the tiny wound. Gradually I worked out this position, and find that it gives the best possible exposure, and enables one, if the assistant is attentive, to perform a very satisfactory suture through the very small incision.
Preparation.
The patient is placed on his back on the table, and small sand bags or folded sheets are put under the shoulder blade and corresponding hip. This slightly raises the shoulder. It is well to draw the patient as close to the edge of the table as may be, so that when desired the elbow can be pushed backwards below the plane of the table—a maneuver which may be needed to expose the upper part of the bursa. The patient's face should be turned toward the opposite shoulder, and the anaesthetist and patient's head protected with a "goiter apron" tied around the patient's neck.
I always arrange a sterile dressing over the hand and forearm, so that during the operation the arm may be manipulated by the operator or assistants. A convenient way is to sterilize the shoulder and arm to below the elbow, and then to draw a sterile pillow slip over the hand, forearm and elbow, and attach it with sterile bandages as high on the upper arm as desired. The arm may then be drawn through the hole in a laparotomy sheet, and moved about at any stage of the operation.
Position of Incision.
In deciding on the point at which to incise, one must Temember that the skin incision will remain stationary, and that by rotation of the humerus the point at which the calcified deposit lies may be brought beneath the incision. The deltoid muscle, which forms the bulk of the tissue which must be cut through, also remains nearly completely fixed. It moves a negligible amount when the humerus is rotated. One must remember also that the sides of the subdeltoid portion of the bursa move considerably in rotation of the humerus. For instance, having incised the skin and muscle, it is possible to continue the incision in such a manner that it would be entirely outside of the bursa; i.e., it might not penetrate the bursa at all when the arm is in extreme internal rotation, but if the cut were made with the arm in external rotation, the bursa would be opened. To make the operation easy, one would desire to have the skin incision as nearly opposite the calcified deposit in the base of the bursa as possible. I have found that the incision best on the average is directly anterior to the head of the humerus, with its upper end near the acromio-clavicular joint, and its lower end at about the level of the top of the bicipital groove. In thin subjects one can feel the bicipital groove through the deltoid, and it is always well to do this if possible, because the acutely tender point will lie external or internal to the groove, according to whether the deposit is in the supraspinatus or subscapularis. The expansions of these two tendons bridge the bicipital groove, but their real attachments are to the greater and lesser tuberosities on each side of the groove. I have sometimes seen the deposit apparently over the groove, but it had probably extended from the tendon on one side or the other.
If one cannot feel the groove before making the incision, one can always determine its position by palpation in the wound after the deltoid has been incised. It is well to do this in every case, for often the exact location of the deposit can be made previously by X-ray, and one can readily locate the subscapularis and supraspinatus if the groove is determined. Sometimes the floor of the bursa does not show sufficient indication of the deposit to guide the surgeon. In such a case the tip of either tuberosity may be readily determined with the point of the knife, and the tendon incised just above it. When a little of the white deposit appears, the incision can be enlarged in the line of the fibers of the supraspinatus or subscapularis, as the case may be.
In order to determine the position of the bicipital groove, one may take it as a good rule that when the elbow is flexed at a right angle, and the posterior part of the elbow put down on the table at the side of the patient so that the axis of the forearm stands directly vertical to the table, the bicipital groove will be at the most anterior portion of the prominence caused by the head of the humerus. From this point, rotation of the forearm either way brings the tendons into view according to the obvious anatomical arrangement. (Pigs. 6 and 51.)
Incising the Deltoid Muscle.
Separating the fibers of the deltoid muscle is a little more difficult than parting those of the rectus in abdominal incisions, owing to the fact that the fibers of the deltoid are more or less "herringbone" in arrangement. The incision seems to close right up on withdrawal of the knife, so that it is difficult to find the line again. I therefore usually put another instrument, as the point of a hemostat, in along the knife before withdrawing it, so that with my knife in my right hand and the hemostat in my left, I push the fibers apart as the assistant places two aneurism needles as retractors to take the places of my two instruments. These hold the line of incision, and the fibers of the deltoid are cut upward and downward to equal the length of the skin incision. Small, broader retractors are then introduced, exposing the upper surface of the roof of the bursa.
If the above has been understood, it will be seen that the skin incision and the deltoid incision are simple and standard. If correctly placed they would lie over the very top of the bicipital groove in the above-mentioned position, with the forearm vertical to the table. It is by no means necessary to hold the arm in this position while the skin and muscle are incised, but when the bursa is to be opened, the arm should be held in this position, the assistant being ready to rotate it one way or the other as the surgeon desires. Make sure that this point is understood.
.jpg)
.jpg)
This figure should be studied with the last one, although for convenience the patient is here represented as standing up while the operator looks downward from above, and the assistant, holding the elbow at the side, rotates the forearm and consequently the humerus beneath the wound. The figures below represent the incision and its relation to the bicipital groove as the humerus is rotated. The Incision remains stationary while the facets of insertion pass beneath the incision. A thorough understanding of these two diagrams is most important.
Incising the Bursa.
The incision in the deltoid having been made, and the fibers retracted, it is well for the assistant to rotate the arm, and in most cases the roof of the bursa is so transparent that the base beneath it can be seen to move as the arm is rotated. In cases in which the bursal wall is thickened from old inflammation, one cannot see through it, but one can palpate the tuberosities moving beneath it. Since it is important not to allow any blood to enter the bursa, small sponges should be ready.
It is well to tie up vessels before making the incision into the bursa, for if blood fills it, it is harder to determine the appearance of the base. At this stage the roof of the bursa is picked up with two pairs of forceps, as is customary when incising the peritoneum. A cut is made between the two forceps, and the air rushes into the bursa, so that the incision can then be enlarged upward and downward as desired. A normal bursa has a white, shiny floor, but a circular zone of deep red injected tissue is usually the guide to the area where a deposit lies. This deep red tissue, resembling that of a bloodshot eye, surrounds a white or pale area about one-half the size of a ten cent piece. Sometimes this area is obviously under tension and mounded up like a boil. At other times when the inflammation is less, the affected area is not raised, and there is only a barely perceptible whitening where the calcium deposit shows through the synovial floor of the bursa. Before incising this area it is well to look the rest of the bursa over, to make sure that there are no other lesions. The X-ray will probably have already determined whether there is more than one deposit, but even if the X-ray does not show more than one deposit, there may be a second one, so that in case of doubt, I believe it is better to prick any suspected area with the point of a knife. I have done this many times, and have seen no variation which could be attributed to this practice in the convalescence of these patients. Sometimes such exploratory punctures of the tendons have fortunately led to the finding of a second deposit, for the patient may suffer an attack of inflammation about one deposit, and then later have another attack due to inflammation about another deposit. While immediate attention to the inflamed deposit is the most important thing, it is desirable when possible to remove or free any other deposit. I recall few cases of deposits which were not surrounded by red zones.
Experience has shown that we rarely find any lesion of the bursa except at the points close to the attachments of the tendons, and these points may all be inspected by simply rotating the arm through its full arc while the wound is held open. It is a little harder to see the extreme edges upward and downward, but practically the whole bursa may be inspected by merely rotating the arm. Pushing the elbow backward (dorsal flexion) tends to demonstrate the upper edge, and pushing it forward reveals the lower limits of the bursa. I have never recognized any lesion of the roof of the bursa. Lesions at the attachment of the supraspinatus are the most common, those at the attachment of the infraspinatus next, and those of the attachment of the subscapularis perhaps a little less common. This relative frequency also holds good in regard to traumatic rupture of these tendons. One must remember that the three tendons are closely incorporated at their attachments, and that these attachments to some extent overlap.
Removing the Deposit.
To return to the operative technique—we may assume that we have reached the point of incising a calcified deposit which we have found in the supraspinatus tendon. According to the stage of the pathologic process, whether acute or chronic, the calcified mass will be softer or harder; in the earlier stages it is little more than a milky fluid; in the older stages it is hard and gritty, coherent and sometimes encapsulated. In most cases it is of the consistency of ointment; often it resembles the contents of a wen. On incision this material usually escapes as if under tension. Sometimes this is very striking. A little nick is made, and there emerges a ribbon of whitish material just as one sees when a tube of zinc oxide ointment is squeezed. Sometimes, however, there is not much tension, particularly in the old cases, and the particles of calcareous matter seem to be incorporated in the substance of the tendon so that they cannot be curetted out without removing shreds of tendon with them. Occasionally the material occupies a well-formed pocket, and one gets the impression that it is wholly removed with the curette. I have oftentimes been content with merely incising one of these pockets, making no effort to curette out all of the material. The symptoms have disappeared quite as satisfactorily as in cases where a thorough curetting was done. Some surgeons, notably Brickner and Harbin, have stated that they excised all the calcified material. I am sure that if they do this, they will remove a considerable amount of tendinous substance which will be replaced with very little scar tissue, so that the tendon will be much weaker. I have sometimes thought that possibly cases of rupture of the supraspinatus tendon from trauma may be particularly common in cases which have had previous attacks of this so-called calcified bursitis, which has weakened the tendon. At any rate, I feel that it is well to do as little damage to the tendons as possible. Attempts to "excise the bursa" are absurd and indicate an entire lack of knowledge of the local anatomy, physiology and pathology.
Closing Incision.
Having removed with the curette the major portion of the deposit, I wipe the cavity out, but do not attempt to sew up the incision in the tendon or in the bursa. Most other writers have recommended that the roof of the bursa be sutured. I have rarely done this, believing that it is better to allow the fluid formed by the synovial secretion of the bursal walls to seep into the areolar tissue. This would naturally wash out any particles of calcium and blood which remained in the bursa. If the bursa is closed these particles might cause adhesions, and perpetuate inflammation. Then, too, in a few cases in which I have closed the bursa, I think there has been more postoperative pain, due to distention of the bursa with blood and serum. I have not found that the adhesions due to the incision healing down to the tuberosity cause any permanent restriction of motion. It appears that the bursa itself reforms as a rule, perhaps not as a simple space, but as several small spaces.
I close the muscle with a few loose catgut stitches, because I have found that unless I do so the wound eventually heals with a depression between the fibers of the deltoid. Therefore, it is better to see that the deltoid muscle returns to its normal contour. Perhaps it is better to close the roof of the bursa, but it would need a considerable number of cases to prove it, for my experience is sufficient to show that it is certainly not necessary. It may add some slight shred of advantage, but I think not. The skin is closed as in any other surgical wound.
Postoperative Treatment.
After the operation I treat the patient just as I would a normal person who had a similar wound caused by an accident. The arm is carried in a sling most of the time for a few days. In about a week or ten days the patient can use the arm in a gingerly way, and can manage to dress himself, and use a knife and fork. Discarding the sling, I then encourage "swinging exercises" in a stooping position. When these become free the "standing exercises" are prescribed. In from three to six weeks the patient should be well, except for occasional twinges of pain and soreness and slight restriction in extreme degrees of motion. These twinges of pain are not severe or incapacitating, and I suppose are due to the irregular contours of the bursal surfaces after the incision. They slowly disappear. My tendency is to allow any free use which does not cause pain.
Finer Points and Occasional Obstacles in the Operation.
In ladies it is well to have the patient try on a low-neclced dress, and to make the incision at a point where the scar will be concealed by the shoulder strap. Since rotation of the humerus covers a considerable arc, the site of the skin incision can be varied a good deal. I have tried a horizontal incision once, but the scar seemed to have a tendency to stretch more than does a vertical one.
I want to repeat that it is important to tie all bleeding vessels before opening the bursa. The blood supply of the skin on the point of the shoulder is very active, and this is increased in cases of longstanding inflammation. Many small vessels sometimes have to be clamped to obtain a dry field. At the extreme upper angle of the wound there is one which is especially annoying, for it retracts into the muscle and readily drips into the open bursa, obscuring the field. As the wound is deep and small, even a little blood causes delay.
Incising the bursa itself may prove confusing, especially where there are adhesions. Normally the roof of the bursa is even thinner and more delicate than the normal peritoneum, but where there has been inflammation in the bursa, it may be as thick as blotting paper, and quite opaque, so that it is hard to see the floor rotate beneath it as the arm is moved. In such cases one usually finds straw-colored fluid in the bursa. In some cases where the deposit has broken through into the bursa, flecks of deposit in sheets of fibrin or milky fluid will be found in the bursa. Such cases would probably get well without operating.
It is not easy to open the bursa in some cases or even to know when your knife has passed through it into the areolar tissue in the nictitating folds. In case confusion arises, keep the arm in the position advised with the forearm vertical to the table, and cut down on the outer lip of the bicipital groove at its upper extremity. Do not cut directly on the bicipital groove, for you might unnecessarily open the sac about the tendon, if the bursal surfaces were adherent. This would probably do no harm, for in the cases of exploration for a ruptured biceps tendon I do not hesitate to do this and have had no unpleasant results. However, it does not help to locate the bursa, so it is best to recognize the groove by palpation before incising.
Adhesions of the surfaces of the bursa may make it difficult to open. In two cases I have opened directly into the space containing the deposit, passing through the two adherent surfaces of the bursa without separating them. Such an experience might give the impression that the deposit was in the bursa. In my experience adhesions are not the rule. They vary, when present, from recent film-like strands hardly more solid than fibrin to dense scar tissue which effectually prevents rotation. As a rule, one readily opens into a good, large bursa, and the white or yellowish deposit surrounded by the turgid, red zone is as conspicuous as it well can be. The confusion comes in long-standing cases when the acute inflammation has subsided, and is replaced by firm, relatively bloodless adhesions about a very small deposit.
It is quite possible that in cases where the deposit is in the subscapulars, a quicker and smoother convalescence might be obtained by pushing the bursa up from below, or from the inner side, and removing the deposit from beneath it without opening the bursa at all. This would leave a smooth bursa, and avoid the twinges of pain which the roughened surfaces produce if the bursa has been opened. I have done this in one case. However, it is surer and safer in most cases to incise directly into the bursa, and be guided by the red zone.
Remember that when the incision is once made, only gentle retraction is necessary. Rotation of the humerus, by using the forearm flexed at a right angle, should take the place of retraction of the lips of the wound. It would be unfair to a patient to attempt to open his bursa unless the meaning of the above sentence was clearly understood. (Fig. 516.)
I have operated on a few cases after the calcified material has perforated into the bursa, but I think now that these operations were probably unnecessary. So many similar cases have promptly got well without any treatment, that I suspect that although my operated cases also promptly got well, the operations had little to do with the recovery. In opening the bursa in these cases a few days after the perforation, I have found a film of whitish fibrin between the two bursal surfaces. Under the microscope little particles of calcium were found thickly scattered through the fibrin, accounting for its whitish look. Recently I have seen two such cases demonstrated by X-ray, on which I did not operate, and the symptoms cleared up as promptly as if I had removed the fibrin.
It seems to me that the time when operation is most indicated is when the deposit has begun to cause subacute symptoms and has not yet perforated. It is in such cases that the mound on the base of the bursa is found, and from which the white material exudes as soon as it is punctured.
I am inclined to think that spontaneous perforation will by nature relieve the symptoms in a few weeks, although it brings on the acute symptoms during the first few days. Operation, diathermy, puncture, injection of proteids, violet light or other treatment may easily get the credit for the good result. It seems a pity that comparative series of such cases treated by different methods cannot be arranged and controlled by a series of untreated cases. It is at least a comfort to know that all the cases under any treatment get well. The object of treatment is only to find the easiest, quickest, and most comfortable way.
My feeling at present is that when the X-ray shows that the deposit has become diffused in the bursa it is unnecessary to operate, unless the quantity is great, as in Fig. 44. One can tell that it has become diffused if the film shows that the deposit lies outside of the tuberosity and, vice versa, if it lies within the contour of one of the tendons it cannot be in the bursa. (See Plate II.)
Sometimes after perforation a portion of the deposit remains in the pocket in the tendon, and this gives a "shirt-stud" shadow in the X-ray.
Be on your guard in interpreting the shadow cast by the bursa with a film of fibrin in it containing the diffused particles. Remember that the bursa is a very thin concavo-convex space, and therefore the mass of material in a lateral view seems greater than it really is. (See Fig. 45.)
OPERATIVE TREATMENT OF RUPTURE OF THE SUPRASPINATUS
TENDON
The best time to operate would be immediately after the injury. When in doubt of the diagnosis, exploratory incision of the bursa should be done. The technique of this incision is the same as that which has just been described for use in cases of calcified deposits. Practically the whole base of the bursa can be inspected through this incision and the exact extent of the rupture determined. The incision is then enlarged inward or outward at either end for a half-inch, depending on the direction of the tear. On account of the herringbone structure of the deltoid it makes little difference whether or not the enlargement of the incision is at an angle with the first one. A good exposure can be obtained with an incision one and one- half to two inches in length. Do not enlarge upward farther than the coraco-acromial ligament.
Assuming that the operation is done soon after the accident, it would seem that no special directions would be needed. The surgeon knowing the normal relations would restore them by appropriate sutures and close the wound in his favorite manner. It seems to me that this immediate operation would be very easy, but I have not been able to operate on one of these cases in an early stage.
In general the operation has two main objects: the repair of the tendon to give power to the arm, and the making of a frictionless lower bursal surface to relieve inflammation and pain. Perhaps the latter is more important, for even a powerful arm, if painful, is not as useful as an arm which is rather weak in the power of abduction but not painful. It is important to keep these two objects in mind, for although in some cases both can be attained, it is sometimes necessary to take a choice between them, because the tissues may be so damaged and retracted that good approximation is impossible. In such a case we may wish to discard all hope of restoring power and devote our whole effort to trying to allay friction. For instance, the tuberosity could be excised wherever it is free from tendinous attachment, and hence is useless. This might diminish the pain by removing the eminence.
One must not feel too discouraged, however, about his repair work, for on several occasions I have opened a bursa a second time and found a smooth base and no visible sign of my suture, which, at the end of my previous operation, had appeared rough and clumsy with the ends of the tendons not even approximated but held "a distance." (See p. 245.) Even in a certain number of the delayed cases which I have operated upon, there has been little difficulty in making a satisfactory suture aiming for both objectives, but in other cases, there was little or no hope of making a smooth, even suture which would leave no rough eminence or sulcus. The latter is particularly likely to be the case where the tendon is evulsed from the tuberosity, leaving no stub to hold the stitches. In a few cases the retraction was so great that no suture could be attempted at all.
Special Points and Special Difficulties
I have found that in the old cases on which I have operated, it is seldom easy, often difficult and sometimes impossible to repair the tendon. It seems best to list the difficulties and then to discuss each.
- Position on table
- Mobilizing the tendons
- The long head of the biceps.
- Drilling the tuberosity or removing it.
- Suturing the rent.
- Formation of a new sulcus.
- Frictionless surface
- Material of suture.
- Shape of needles.
- Closure of bursa. Disposal of fluid.
- Postoperative treatment.
1. The arrangement of the position of the patient on the table to permit proper mobilization of the arm during the operation, is an important factor in technique. The point of the shouldeT is a difficult region on which to work, for both the surgeon and the assistants. It slinks away and the patient's head and neck seem to wish to take its place. (See Fig. 50.) I should like to stress the importance of so placing a heavy sand bag under the shoulder and another under the corresponding hip that the patient is half turned on his side, while the head, with the face turned away, is at a lower level than the point of the shoulder. The shoulder should be slightly over the edge of the table toward the operator, so that the arm may be allowed to hang down in a position of dorsal flexion when desired. This position throws the distal portion of the supraspinatus tendon forward for the maximum distance from under the acromion.
The operator and assistant stand on the same side of the table, while the anaesthetist and nurse with the instrument table are on the other side. A second assistant is welcome, and often almost necessary, because the first assistant must at times give his entire attention to holding the arm and the nurse may be occupied with retractors. Much of the facility with which the operation is conducted depends on the assistant who holds the arm, for his ability to rotate just at the right time will enable the operator to put his needle at just the right point in the somewhat small field. Since the lips of the incision do not move appreciably, the operative field is really controlled by the assistant as he rotates the humerus, bringing this side of the rent or that into a position which the operator desires.
The maneuver already described, of letting air into the joint and bursa, is often a great help. The position in which to place the sutures is best illustrated by a diagram. (Fig. 52.) While this is the ideal, it is seldom possible to carry it out exactly, for too often the retracted, stiffened tissues cannot be worked into nice apposition.
.jpg)
FIGURE 52. METHODS OF PLACING SUTURES
a illustrates the writer's suggestion that the biceps tendon may be sutured to the supraspinatus in some cases when the former has been already torn from the edge of the glenoid, b, c, and d suggest the method of placing the sutures in the ruptured supraspinatus and in the tuberosity. The ideal is c, for in this case the lines of incision have been carried up on each side of the supraspinatus to mobilize it. d illustrates Dr. Wilson's method of cutting a slot to receive the supraspinatus tendon, e and / offer a suggestion for operation in a case where the short rotators have been entirely evulsed from the head of the humerus. Fascia lata might be passed through a drill hole and through a slot over the tuberosity to form an anchorage for the tendons.
2. Mobilizing the tendons. When one considers that each one of the short rotators is separated from the other by a definite bony partition through most of its extent, and it is only the last three-quarter inch which is welded with the others into the terminal conjoined tendon or cuff (Fig. 10), it would seem easy to isolate any one tendon so that the more or less elastic muscle belly could be stretched enough to bring the tendon down again to the tuberosity and suture it there. However, if you try this on a normal shoulder at autopsy, you will find it is not easy, and when you try it on a ruptured tendon in which operation has been delayed for many months, you will find it impossible.
In the first place, you are cramped for room by the acromion and coraco-acromial ligament so that you cannot see the muscle bellies even in the normal shoulder. In the second place, if you dissect back more than an inch on either the supraspinatus or infraspinatus, you run the risk of wounding the suprascapular nerve, and if you do, you may lose your power in those muscles forever.
In order to get at these tendons more effectively, I used to use the "sabre-cut incision," which gave a perfect exposure and every possible opportunity. (Plate VIII.) Even then the mobilization was only a little more satisfactory, so I have given up this incision. Practice has given me a little more confidence, and I believe now I can do almost as well through the simple routine incision. Dr. William Rogers has suggested removing the deltoid attachment with the periosteum from the acromion and suturing them back at the end of the operation." This seems rational, but I have not tried it and do not know whether one may rely on having the deltoid origin anchor again satisfactorily. I have sometimes thought that a subcutaneous osteotomy of the base of the acromion might mobilize it enough even without division of the coraco-acromial and acromioclavicular ligaments to allow easy access. The trouble with any incision which mobilizes the acromion is the long period which one must wait for union to occur before moving the joint. I am inclined at present to do all the mobilizing I can through the routine incision, and I find that I am constantly improving in my ability to do this.
It is probably best to remove the falciform edge of new tissue and to refresh the edges of the tendon itself. I attribute some of my imperfect results to my failure to do this. One learns by experience to put the suture back of the falciform edge, for the latter has no strength and the stitch at once tears out. One is tempted not to remove the edge because it is obviously difficult to close the rent without using it, and it seems folly not to save all the tissue one can. It might be contended that the falciform edge may have more tendency to unite than the real tendon substance, which has very little blood supply, so that perhaps I may be wrong in recommending the removal of this new tissue with which nature is attempting to repair the damage. The method of closure which seems to me the best is illustrated in Fig. 52.
3. The long head of the biceps. The problems connected with how to deal with the long head of the biceps when it is found exposed, owing to the retraction of the ruptured tendons, are not a few. I can only discuss them and do not pretend to solve them. Although I am not in agreement with some of Meyers' views on the importance of the role of the biceps tendon in shoulder injuries, I feel that his observations ought to be known to every one who operates on these cases. To my mind, the rupture of the supraspinatus is the primary and important lesion which uncovers the biceps tendon, makes it slip a little at the top of the bicipital groove and to tend to be caught between the tuberosity and the acromion. At any rate, one often finds it a conspicuous, pink, inflamed-looking, swollen band lying across the j oint cartilage at the bottom of the rent. ( Plate VIII.) The portions exposed in the rent look inflamed; those covered by the remaining intact part of the capsule are white, glistening and normal. It is pretty obvious that our suture should cover up the biceps tendon without interfering with it otherwise. It usually lies just under the inner edge of the rent, but if any of the subscapularis fibers are involved, it lies entirely exposed. Sometimes it is not found at all, for it has been torn away from its glenoid attachment and has retracted down the bicipital groove. Sometimes it is split in two, longitudinally. Often it is flattened and frayed at the edges. Varying proportions of it may be ruptured. It may be composed of indefinitely separated longitudinal strands, some of which have become welded into the capsule. It may have little, rice-like tags on its edge. However, almost always the parts which do not become exposed in the gap left by the supraspinatus are normal in appearance.
When it has ruptured from the glenoid, it may be held high in the groove by a few remaining bands, and we can capture it and pull it up. What shall we do with it? We might try to suture it back on the glenoid, or rather on the fibrocartilage which surrounds the glenoid. Or we might attach it to the proximal portion of the supraspinatus, or to the capsule, or anchor it in the groove, or excise a part of it and use it to repair the supraspinatus. We might even take a relatively normal biceps tendon, clip its attachment off the glenoid, anchor the tendon in the groove, and then use the redundant portion to fill the gap in the supraspinatus. (Fig. 52a.) This would give the biceps muscle a fixed origin, and we would at the same time obtain a firm attachment for our supraspinatus. We should only have lost whatever function the long head of the biceps has from having its attachment on the glenoid rather than on the humeral head; i.e., the outer head of the biceps would no longer be of use in motions of the humerus on the scapula, but could still apply its power in flexing the forearm on the humerus. What then is this function which we should lose so far as scapulo-humeral motion is concerned?
The function of the biceps muscle is fourfold. First, it is a flexor of the forearm on the humerus. Second, it is one of the flexors (or extensors?) of the whole arm on the scapula; in a sense, therefore, it is a weak abductor or elevator of the arm. Third, the external insertion on the tubercle of the radius enables it to act as a supinator of the radius and hand. Fourth, the long head of the biceps passing through the intertubercular groove helps to retain the head of the bone on the glenoid, and stabilizes the head in the various degrees of rotation, as the arm is elevated. This function is well illustrated by the findings in two of my cases, which at operation showed that except for the subscapularis, the whole of the capsule with the tendons of the supraspinatus, infraspinatus and teres minor had been evulsed, yet the head did not tend to dislocate; apparently it was held in the joint'by the long head of the biceps, and by that only. We lose nothing in the first function, little in the second, none in the third and but a problematic amount in the fourth, by using it in the way suggested in Fig. 52a.
So far as the action of the shoulder joint is concerned, particularly with reference to the functions of flexion of the arm on the scapula and of the forearm on the humerus, the origin of the short head of the biceps from the coracoid process is more important than that of the long head from the edge of the glenoid. The coracoid origin is sufficient to give power in these motions; the long head is chiefly a stabilizer and one of secondary use so far as the application of power is concerned. For instance, in cases in which the long head of the biceps is ruptured and no other lesion has occurred, the function of the shoulder remains almost normal.
The short rotators are sufficient to maintain the fulcrum on the glenoid in most positions of the arm, but where these short rotators are damaged, I am confident that the long head serves a very useful purpose in guiding the head of the humerus and restraining it from forging upward and getting its fulcrum on the acromion. I therefore regard it as important to keep the long head of the biceps intact if possible.
I have notes that in some of my operated cases, the biceps was torn away from its glenoid attachment. In such cases in future I intend to search for the distal end of the tendon and to anchor it with stitches in the bicipital groove, and also to the supraspinatus tendon, thus abandoning any idea of retaining its stabilizing function and being content with retaining its power as a flexor of the forearm. At present I see no good mechanical way of re-attaching it to the glenoid so as to make it function in guiding the head of the humerus as the latter is abducted. One is apt to think of the long head of the biceps moving up and down in the intertubercular groove, but this is not what actually happens. The humerus moves up and down on the tendon; it is not the tendon which moves through the groove. (See Fig. 52.) On the whole, I should say that if the operator finds that the biceps is so damaged that he thinks it will not in future form a smooth cord on which the humerus can ride up and down, he had better use it, as described above, to replace the lost substance in the supraspinatus.
4. What shall we do if we find there is no stub of supraspinatus tendon left on the tuberosity to which we may suture the proximal portion? In long-standing cases we find a tuberosity completely bare of tendinous substance, and perhaps somewhat eroded. Since this tuberosity is useless unless we can suture the tendon to it, it might as well be removed. I have not hitherto excised the tuberosity in cases in which I could not suture, but it might be well to do so. Such an excision would make the surface which must ride under the acromion less apt to cause friction. Nature does exactly this by causing recession of the tuberosity. As a rule I have drilled two holes in the tuberosity with an ordinary shoemaker's awl, and passed a heavy silk suture through these holes and the tendon so as to draw the tendon as nearly as possible to the facet of insertion of the supraspinatus. This can usually be accomplished, but occasionally the supraspinatus is so retracted that I cannot quite draw it down to the bone.
I have on several occasions made a sort of plastic so that I covered the suture with part of the roof of the bursa, believing that the repair of the tendon comes not from the tendon itself, but from the adj acent synovial membrane which is much richer in vascular supply.
5. Another operative problem is how to repair the rent. As explained in the chapter on pathology, these rents are in a general way triangular, with the base on the humerus and the apex retracted, the apex being usually the center of the supraspinatus, and the sides the lateral expansions which are united to the neighboring tendons. The ideal way to close would be to bring the center of the apex to the center of the base, but if the retraction is great and the base is small, the triangle is so prolonged upwards that one is tempted to close the gap from side to side until very near the base, and then to make
the last suture a triangular stitch. This method is easier, but it does not bring back the normal relations. However, it is a feasible method to use where there is much retraction. The exact way in which to put the sutures does not seem important, that is, whether they are mattress sutures or interrupted or continuous.
6. Formation of a new sulcus. If the reader will refer to Chapter IV, and especially to Plate VI, Figs. 3-4, and their legends concerning the remarkably effective method which nature has devised to attach the supraspinatus tendon to its facet, he will feel great doubt as to whether the surgeon will ever be able to imitate it with any degree of success. We need much study and experimental work before we can rely on being able to create a line of living cement such as the "blue line," with its pores for the finger-like processes. At present, from what we know of histology, it seems doubtful
whether in adult life such a method of union of tendon to bone can ever be achieved. However, we know that tendon can form a fairly firm cicatricial attachment to raw bone. What is the best practical way to secure this ?
If it were possible, we should wish to have the new tendon form on the raw surfaces of the sulcus and of the tuberosity down to the actual edge of the joint cartilage. When I drill the tuberosity I try to drill it as far as the cartilage edge, and I usually erode the bone of the sulcus with the point of a knife or curette, so that the tendon will have a little better chance to become attached by granulation. Dr. Philip Wilson has improved on my operation by cutting a slot around the cartilage edge and drilling through the base of the tuberosity. He then passes a slip of fascia lata through the drill holes to be attached above to the supraspinatus. He thus makes a more ideal suture, so that the tendon fills the entire sulcus and thus gains a firm hold on the tuberosity. It remains to be seen whether nature will tolerate such attachments indefinitely.
7. A frictionless surface for the base of the bursa is a most important point. Dr. Wilson's method has this advantage. It would be repetition to discuss this further, but I should like to repeat that even in those cases where the suture at the end of the operation has seemed rough, it may nevertheless be so changed by the healing process that a surface is produced which at a later operation appears smooth and normal.
8. I use silk sutures because I want them to endure long enough for new, strong, scar tissue or tendinous substance to form over them. I use a fairly heavy pedicle silk for the main suture, which passes through the holes in the tuberosity or between the proximal and distal portions of the tendon. I have on four occasions reopened the bursa later to remove these silk stitches because the patient complained of pain. The following are the findings in these four cases:
CASE 18
Mr. R. H. S. Age 60. M. G. H. No. 181765 E. S., Mar. 26, 1912. A typical case of complete rupture of the supraspinatus, one and one-quarter inches wide. Although much retracted, the tendon was caught and sutured in place with three mattress sutures. The functional result was good, but he continued to have more or less pain, apparently from the formation of a considerable amount of dense inflammatory tissue about the site of suture. On Feb. 13,1913, under novocaine, the bursa was again opened and the tendon was found not only completely repaired, but there was a large amount of dense hypertrophic, callous-like tissue about the sutures. This mass impinged on the acromion in abduction; most of it was removed with the scissors and a new opening made through the supraspinatus into the joint, so that some of the synovial fluid could flow into the bursa and lubricate it. The result of this operation has been satisfactory. Twelve years later, on June 9, 1925, he called to see me because of a slight injury to his left shoulder. The right, on which I had operated, had given him no trouble in the intervening years, although he had worked steadily as a coachman.
CASE 29
Mr. M. M. W. Age 39. M. G. H. No. 184216 W. S., Aug. 5, 1912. A clear case of badly ruptured supraspinatus tendon. The tendon was sutured with heavy silk and function was restored. During the following year he had much pain on use of the arm in his work as a laborer. The bursa was again explored and the silk sutures and some of the chronic inflammatory tissues lying about them were removed. I also made a new opening into the true joint to permit the fluid to flow into the bursa. This was followed by improvement but not by complete relief. No late report. Note that entire repair of the rupture had taken place.
CASE 88
Mr. T. M. Age 50+. Operated on at Faulkner Hospital, July 24, 1926, six months after his injury. The supraspinatus, infraspinatus and part of the subscapularis were found to be torn away, exposing the biceps tendon, which was greatly inflamed. There was much fluid in the joint. A very unsatisfactory suture was made, and the tuberosity had to be drilled. The arm was put up in abduction. Mild sepsis occurred and there was much fluid drainage, so that the wound took several weeks to heal. Some of the deep sutures were taken out. In spite of this the result at first was good, and he returned to his work after five months. He worked for a year and three months, although in some pain, and then had another slight injury. On July 2, 1928,1 again explored the bursa and found that most of the sutures had pulled away, leaving the condition practically as bad as at the first operation. This was as bad a result as I have ever had. The patient was for a time benefited, but in the end gained nothing by the operation, for I did not attempt a second suture.
CASE 112
Mr. A. C. Age 62. Operated on at the Trumbull Hospital on June 11, 1928, three months after his injury. A typical complete rupture of the supraspinatus was found and satisfactorily sutured. The immediate result appeared to be good. However, the patient would not go to work again, complained bitterly of pain on use of the arm and became very neurasthenic. On Feb. 7, 1929, I again explored the bursa, thinking that if I took out the deep sutures some of the irritation might be relieved. My notes say:
"I operated on him yesterday under novocaine ansesthesia. Dr. B. E. Wood was present and Dr. Stevenson assisted. Incision was made just inside the old scar and the bursa was opened. It was clearly shown that the former suture had been effective in restoring the insertion of the tendon. Moreover, the floor of the bursa was smooth and shiny, and there did not appear to be any cause for friction over the site of the suture. One heavy silk suture could be seen just below the transparent synovial lining of the base of the bursa; this was easily pulled out, but the other two sutures were buried deeply in the new-formed tendon and were found and removed with difficulty, as I was anxious not to weaken the tendon in so doing. In two of the sutures the knots were apparently untied; in one the knot was still present, but almost untied. At first I thought that the knots of the two untied ones had been left behind, but on reflection I think it is more reasonable to suppose that they had become untied as the tissues increased in amount and grew into the knots, which were cut very short. Yet it is possible that they broke off and remained in, although the total amount of silk in the untied ones appears greater than in the tied one by more than double. At any rate, very little silk could have been left behind.
"I did not feel satisfied that the silk was causing any trouble, for there appeared to be no inflammation about it, and the tender point of which the patient complained was nearly a half-inch away from the sutures, on the edge of the greater tuberosity close to the bicipital groove. That there was some inflammation at this point was made clear by finding a little crumbly, soft, cheesy tissue close to the synovial sheath of the biceps tendon, which in certain positions bulged slightly. The repair of the tendon was weakest at this point, and I fear that my search for the sutures weakened it still more, although not to an extent sufficient to interfere with function, and recompensed by the finding of this suspicious tissue. Two tiny bits of this tissue were saved for pathologic examination. (Plate V, Fig. 5.) The patient still claimed to be unable to work in January, 1931.
Since three out of four cases, which were explored a year or so after the first operation, showed not only firm tendons but hyper-trophied ones, it seems to me that it is proved that suture may be effective. In each case I was surprised to see how well nature had restored the even convexity of the floors of the bursae, which at the completions of the operations had been quite irregular and rough at the suture lines. All four cases, if operated on immediately after their injuries, might have had excellent results; as it was, although two of the four cases had good results, little was gained by the other two patients, unless they may take some satisfaction as demonstrators of the fact that these tendons even when badly broken may be repaired.
9. The shape of the needles is dictated by the shape of the field of operation and by the fact that a tremendous strain is put on them. They must be either fully curved or half curved, not over a half-inch long and with very strong shank and eye. One has to
work between the acromion and the tuberosity, where there is very little room, so that even a curved needle such as is used in ordinary operations is too large to be turned about in this space.
10. Shall we close the roof of the bursa or shall we merely close the muscle, leaving the roof of the bursa free to allow the synovial secretions to seep into the areolar tissue?
As I have previously stated, there is usually in these cases a considerable synovitis with a large amount of fluid. If the bursa is closed tight, this fluid forms under tension and causes pain. Closure also tends to keep blood in the bursa which would otherwise be washed out by the fluid itself. I prefer the idea of leaving the roof of the bursa unsutured to allow this fluid to escape, but I am not prepared to say positively that it is not better to suture the bursa and allow free motion after the operation to pump fluid out between the stitches. The fact is, in cases where there is much fluid (and these cases are usually those that have continued to work in spite of the friction and pain), the fluid seeps into the soft tissues to an extent which causes marked swelling and sometimes induces an edema and suggestion of sepsis. This used to be a frequent complication when I put the arm in elevation, permitting the lower side of the capsule to be held tense and therefore driving the fluid up toward the wound. Now that I treat them without restraint, I do not have this complication
11. The postoperative treatment. I find that my tendency has been, as the years go by, to allow more motion and to allow it sooner. I usually pad the axilla with a small pillow and then let the arm lie on it in a position a little more abducted than that in which the arm rests in a sling, contriving as best I can to keep the hand away from the front of the abdomen, because the tendency of the patient after these operations is to get the arm in a strongly internally rotated position, and therefore the recovery of the power of external rotation is slow. After the first night is over, I remove the dressing and let the patient put the arm in any comfortable position which he can find. Each day I exercise it in a way which is difficult to describe, but which is a matter of personal touch. The general purpose of the exercises is to let the patient bend his body from the hips with the arm relaxed, as described under the stooping exercises (Fig. 47). As in treating fractures near joints, I try to make the patient do as much active and passive motion of the arm as I believe I can without displacing the fragments. It is impossible to lay down more definite directions, but I may say that by the end of the first week I expect the patient to be able to bend his body at the hips to a right angle, and to let both the injured and well arm fall in a relaxed position at right angles to his body. By twisting his body from side to side so as to make one shoulder higher than the other, alternately, he can also move the joint without contracting the shoulder muscles. During the second week he is encouraged to swing the arms a little in both directions in this stooping position. The wound should be soundly and completely healed and the patient discharged from the hospital in from ten days to two weeks. After that he is encouraged to take the stooping exercises.
If the patient is cooperative and understands the mechanics of the operation and can use common sense in taking his exercises, he gets on fairly smoothly, but there is pain of an annoying although not of a serious degree, not only for weeks but for months. I do not think this would be the case where the operation was done immediately after the accident. In convalescence it is a good rule to restrain the patient from exercising his arm in the erect position until he has learned to abduct it freely and strongly in the stooping position. (See Fig. 47.) In long-standing cases the nerves of the region have already become sensitized and are slow in returning to a normal condition. Much of this postoperative soreness in the delayed cases is due to the sensitiveness and synovitis acquired between the date of the injury and that of the operation.
.jpg)
THE SABRE-CUT INCISION
Reprinted from the Bos. Med. & Surg. Jour., Mar. 10, 1927. It does not differ greatly from Kocher's posterior incision, but is more appropriate after a preliminary exploratory cut anterior to the joint.
FIGURE 1
"Sabre-cut" seemed an appropriate name for this incision, for it might well be made by the downward cut of a sabre on top of the shoulder. An incision is made through the acromio-clavicular joint and continued with a saw through the base of the acromion. The anterior point of the incision would be continuous with a previous routine bursal exploratory incision. When the acromion has been sawed through, an epulet of tissue, consisting of the deltoid muscle and the acromion process from which it arises, is formed to be pulled outward and downward. This step is accomplished' with ease, for it is only held by a little areolar tissue and a few fibers of the trapezius attached to the upper margin of the detached portion of the acromion. The upper posterior fibers of the deltoid must be separated a little to gain mobility. In sawing the base of the acromion one must bear in mind the suprascapular nerve which supplies the supra- and infra-spinatus muscles and lies between them, a little below the saw-cut. It is deep enough to be out of the way of the saw but not of gross carelessness.
FIGURE 2
The second diagram shows the structures exposed when this epulet is pulled downward and outward. Even without dissection one can identify the subscapularis, supraspinatus and infraspinatus as they emerge to join together their tendinous expansions beneath the base of the bursa. To one unfamiliar with this dissection the smooth convex surface of this base appears to be the articular surface of the humerus. The subacromial and subcoracoid or coraco-humeral bursse are nicely shown. As explained in previous papers, they are often intercommunicating and are always functionally one bursa although frequently, as in this instance, separated by one of the diaphanous nictitating folds. Notice the separated portion of the acromion and see how easily it will fit back into place.
FIGURE 3
The third diagram is identical with the last except that the supraspinatus and capsule have been cut across into the true joint and the ends of the supraspinatus depicted as retracted. The stub of the tendon is still attached to the tuberosity beneath the base of the bursa, while the muscular belly is retracting into the supraspinatus fossa. The glenoid and the articular surface of the humerus are exposed, with the long head of the biceps arising from the superior edge of the glenoid lying across the cartilaginous surface of the head of the humerus.
This is exactly the condition I have found at operation again and again in the living, except that there is seldom so much of a stub of tendon still attached to the tuberosity. Quite frequently it is entirely evulsed from the latter, requiring drilling of the tuberosity to resuture it. I have always found the base of the bursa to be torn across with the tendon. The point of least resistance appears to be about the subbursal portion of the tendon. In fact the tendon itself is very short, the muscle fibers beginning within a half-inch of the attachment.
In the long-standing cases on which I have operated the biceps tendon is found inflamed, swollen and bright pink in color, forming a striking contrast with the white articular surface of the humerus. Sometimes it is apparently absent entirely, having been evulsed and then retracted downward into its sheath.
To close this incision the parts are sutured back into place in the reverse order of these diagrams. It is probably safer to wire the acromion process, although catgut in the soft parts holds it well. I do not advise attempting to close the bursa even in the exploratory operation; a stitch or two in the muscle holds the edges in sufficient apposition and excess fluid may drain into the areolar tissue.
The pendulum will probably swing in future toward postoperative treatment in abduction and back again to adduction. Dr. Wilson now uses abduction after the sabre-cut incision and complete repair of the insertion into the bone by the use of fascia lata. It is possible that this method has the advantage of creating a larger gap between the head of the humerus and the acromion and the coraco-acromial ligament, because reunion of the mobilized acromion process would take place at a higher level, since it is pressed upward by the abducted humerus.
The Sabre-Cut Incision. Although I have personally given up the sabre-cut incision for cases of rupture of the supraspinatus, it is still used by others, especially by Dr. Wilson. It gives a splendid opportunity to repair the tendon or any other structure in the shoulder joint, but it is really a major operation, while the one I use is a minor one. The main reasons why I seldom use it are three. In the first place, I have learned to work through the routine incision in such a way that I can do the operation without cutting any ligaments or bone. This improvement has come about not only from doing the operation in dorsal flexion, but by using the method of rotating the humerus so that each desired point is placed in the middle of the small incision at the appropriate moment for a stitch. One assistant has to manipulate the arm in unison with the wishes of the surgeon. In the second place, I have found that after division and suture the acromio-clavicular joint may remain somewhat unstable.
A third reason is less technical and more in the domain of human nature. In Industrial Surgery there is not a frank understanding between surgeon and patient as in their ordinary professional relation. The patient is apt to have the element of compensation too strongly in mind, as compared to a cooperative tendency to make the best of the surgeon's attempt to better an injured limb, although both know it may never again be "as good as new." The extent of the sabre-cut incision exaggerates in the patient's mind the degree of the injury and the scar would certainly be impressive to a commission or jury.
Operations for correction of deformities due to paralysis of the shoulder muscles. There are many interesting operations of the above kind which have been devised and which in some cases in expert hands have been successful, but none may be said to be of sufficiently standardized technique to be considered in this book, especially as I have had no personal experience in such cases. The most encouraging example is the operation recently devised by Dr. Frank R. Ober for the relief of paralysis of the deltoid muscle. (Jour. A. M. A., Dec. 24, 1932, p. 2182.)
I have had the pleasure of seeing the case illustrated by Dr. Ober, and can testify to the ability of the child to raise the arms as indicated by his illustrations. Dr. Ober tells me he has since done a number of other cases with the same encouraging result. The operation consists in a transfer of the origins of the triceps and of the short head of the biceps to new attachments on the acromion process, thus using these muscles as abductors.
NON-OPERATIVE TREATMENT OF RUPTURE OF THE SUPRASPINATUS
TENDON
I think every general surgeon who could see one of the complete cases at operation would agree that no form of physiotherapy could influence beneficially one of these lesions, except in a subjective way. The subjective symptoms might possibly be alleviated to a certain degree by massage or by diathermy, but as a matter of fact, nearly all patients say that these agents are of little help. From the very nature of the lesion, manipulations and forced exercises can do no good and might do some harm. If it is determined that a patient is not to have an operation, there are two rational plans of treatment: (1) Fixation in elevation to relax the tendon, improve the blood supply and approximate the torn ends; (2) Gentle "stooping exercises" to help nature smooth off the irregular surface of the lesion. This is merely an aid to nature's own partially successful method.
Fixation in elevation, to be effective, would necessarily have to be instituted soon after the injury, and would require at least three weeks. It would be useless in old cases, yet even in the old cases one can see, when the bursa is open on the operating table, that there is a tendency toward approximation of the torn ends of the tendon as the arm is abducted. Of course, in these old cases the proximal end is retracted and cicatrized in its retracted position. Even prolonged fixation in such cases could accomplish little except in possibly diminishing the size of the defect. This tendency to approximation observed at operation in old cases, when the arm is abducted, shows that it is probable that if the rupture were small, this treatment, if immediately instituted, would be worth while. If I were the patient, I would prefer incision and suture to this problematical and uncomfortable, even if reasonable, plan.
The "stooping exercise" method is founded on the pathologic findings described in Chapter III. Clearly nature has developed this method of absorption of the tuberosity to restore function after this accident, for as these patients, after a year or two of misery, improve somewhat, it is fairly clear that this method of smoothing off the eminence and sulcus which caused the jog is the best she can do. Nature's plan is the combination of this slow smoothing-off of the tuberosity and meanwhile increasing the supply of fluid, which, as the lower portion of the capsule becomes tense in any action, is forced up to the site of friction.
The idea of the stooping exercises is to begin this process with the weight taken off the arm so that the irregular surface is not forced up under the acromion by muscular tension. If the patient stands and elevates the arm, the very point which is sore becomes the fulcrum on the acromion for the deltoid to exert its power. When the patient stoops with the arm relaxed, the scapula can be abducted on the humerus without the need of the fulcrum either on the glenoid or acromion. Gravity takes the place of the power of the deltoid.
It is clear that until a patient can swing his arms freely in the stooping position without pain, he is not ready to use the arm when standing.
To patients who refuse operation I explain these mechanics and impress on them what I have said in the last paragraph. I also try to teach them to sleep with the arm abducted, with the hand behind the head. Palliatives in the form of drugs or physiotherapy are not often required in these cases. The pain is always bearable, if they do not increase it with work or exercise which make a fulcrum of the sore point. I think I can accomplish more with these patients by explanation of the mechanics of their trouble than I can with any palliative measures. Show a workman the normal function of the joint, the necessity of the supraspinatus to maintain the fulcrum on the glenoid, the tendency, without it, for the fulcrum to ride on the sore spot where it touches the acromion, the changed action of the weight of the arm when stooping or lying with the hand behind the head, and, as a rule, he will get your drift. He knows about levers and weights. When he understands his condition, he will get rid of the fear element and realize that though his arm is impaired, he has not really lost the use of it. He has learned that he has lost the use of certain motions unless he is willing to stand the pain. This education has more therapeutic value than drugs or electrical treatment. Massage, of course, may do good in stimulating the nutrition of the tissues, but it cannot unite the tendon.
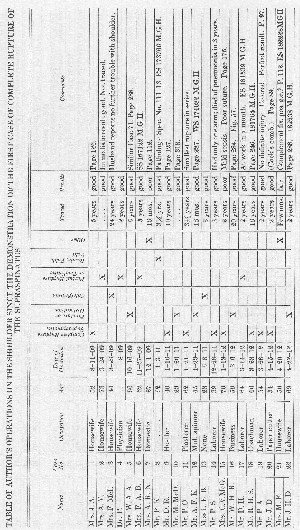
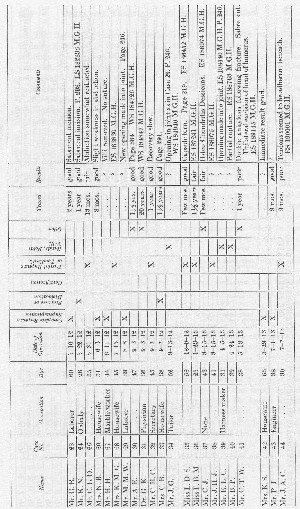
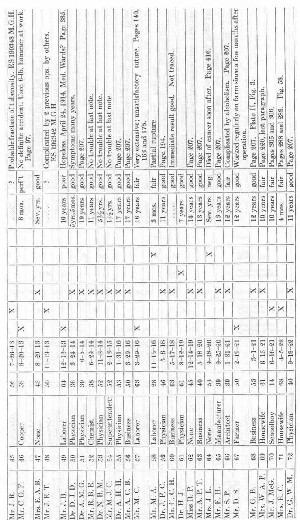
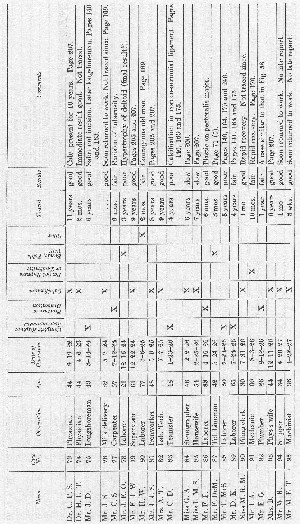
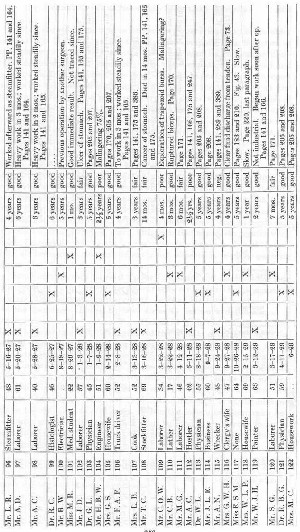
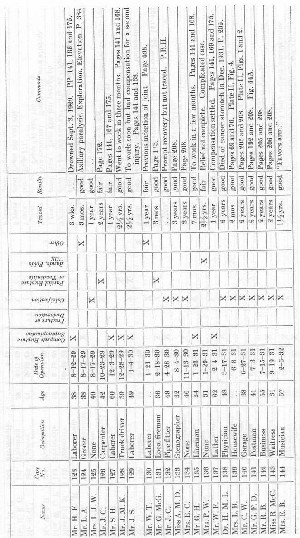
It has seemed to me best to present my operations on the shoulder tabulated in this way, rather than to give complete case histories of each patient. Many of the cases have been used in the text to illustrate different points, sometimes only the occupation being used and perhaps in another place the preoperative diagnosis given to compare with the operative findings, etc. Under the comments at the right of this table the page numbers are given when the individual cases are referred to in the text. Should any one desire to do so, he could, by referring to these pages, make up brief individual case histories. As a rule, the cases which have been spoken of in the text are those in which the result was poor or fair. Those which I have considered good, lack detail. On the whole, compared with the results of the cases in the rest of the table, the outcome in the cases of complete rupture has been relatively poor. The reader is urged to bear in mind that in all the cases on which I have operated my attempts were more or less delayed, for only cases 18, 27, 42, 49,106,115,127, 128, 129 and 135 were done within two months of the accident. In cases 49 and 115 suture was impossible, and cases 27 and 42 could not be traced over a period of years, although the immediate results were good. I probably should not have written this book at all had the results all been good, for one of my chief objects is to urge prompt diagnosis and immediate operation.
Some of the cases marked "poor" actually did obtain some improvement. For instance, Case 88 worked over a year after the operation and then had another accident, so that his total compensation was the maximum allowed by law. Case 89 has worked steadily as a watchman after he had made a settlement with the insurer. I feel that I have certainly not exaggerated the benefits of surgery in these delayed cases, for I am sure something was accomplished in all of them, even in cases such as number 115 where no suture was attempted, for at least a definite diagnosis was made, as a basis for a settlement. If, as I hope, eventually the profession comes to realize the importance and frequency of this lesion, and the laboring class becomes educated to take it seriously, exploration through a small incision will be the rule in doubtful cases. When the insurance companies become interested in the problem, I shall be glad to cooperate in making a more extensive survey of the economic side than that which is presented on page 176.
REFERENCE
Wilson and Fowler have modified my operative methods. References to their articles will be found at the end of Chapter V.


