Brachial Plexus paralysis
CHAPTER XI
BY J. H. STEVENS
[Introduction by Dr. Codman]
IN 1929 when I had already spent a year on this book, I found, by mere chance, that my neighbor, Dr. Stevens, had for a long time made a hobby of studying the brachial plexus. I had often talked with him about other injuries of the shoulder, subjects on which he had made some important contributions, but he had never mentioned that he had been so much occupied with studying lesions of the brachial plexus. I found that he had never written anything on the subject because, after all the years of study he had devoted to it, he felt that little was really known about these lesions and that his personal views would interest very few readers.
I asked him if he would not review his notes and write a chapter for my book. Although he said that he could add very little to the ordinary textbook knowledge about the subject, I assured him that if he did give me the benefit of what study he had made, it would at least bring the subject up to date and show that it was open for still further investigation. I at length persuaded him to try. He had at that time dissected ninety-two plexuses through the courtesy of the Tufts Medical School, and since then, through the kindness of the anatomical department of the Harvard Medical School, he has been able to dissect a good many more, but owing to his illness during part of this time, he was only able to analyze sixteen of these later dissections for this chapter. However, these were done very carefully, with especial reference to confirming his previous observations.
On March 24,1932, Dr. Stevens died suddenly from heart disease, leaving his work in preliminary manuscript form for me to use. The following chapter has been constructed from his manuscript, using largely his own words, but modified to some extent because I was obliged to abbreviate parts of it, and in other parts to add a few paragraphs to clarify his meaning. The substance of the chapter is his and he deserves the credit for all the originality which it contains.
I have used the portions of his manuscript which seemed to me original and enlightening, although in some cases I have not actually verified his observations or presumed to criticize his conclusions. For instance, I have made no dissections to verify the new nerve filament which he describes, nor can I take any stand in regard to his views about prefixed and postfixed plexuses. Neither could I review and tabulate the 710 cases which he has collected and analyzed. I have merely set down his conclusions and can only say that they seem to me valid.
Dr. Stevens was one of the most independent-minded men I have ever known. He practiced surgery for many years in Boston, but was never associated with any of the large clinics. Nevertheless, he was a true student of medicine, and took the greatest interest in his own individual patients. Any case which he could not thoroughly understand led him to study the subjects involved most carefully, not only by searching the literature, but by experimental work in the machine shop or in the dissecting room. He had little respect for modern authority and always tried to trace his subject to the original writers who first described it. For these pioneers in medicine he had the greatest respect and admiration, and a corresponding scorn for plagiarists. As the years went by, his habit of giving intensive study to each obscure case which occurred in his practice, gave him a remarkable all-around knowledge of surgery and its problems. Few men in their fifties and sixties have the industry to dissect out the branches of the brachial plexus to satisfy themselves about mooted points which they have unearthed through finding differences of opinion among famous authors.
He seldom spoke at medical meetings for he was of a retiring disposition, although on superficial acquaintance he seemed assertive. I have never heard him " read a paper," but he published several papers on fractures, which to my mind show an unusually clear grasp of the subjects. It was very characteristic of him to have done all this work and more on the plexus and to have made no attempt to publish it. He enjoyed satisfying his own curiosity, but he hated the details of publication. I feel that I was very fortunate in being able to rescue from oblivion some of the thoughts suggested by his investigations. At any rate, I believe that the surgeon who is willing to give proper study to this chapter will agree with me on finishing it, that he has a clearer and better idea of brachial plexus injuries than he ever had before. One feels that the subject has been very carefully studied by the author, and that his views about the essential mechanics governing these injuries have been thoughtfully presented,
and are not likely to be challenged.
E. A. C.
CAUSES OF BRACHIAL PLEXUS PARALYSIS
1. Traction.
a. Birth cases.
b. Blows on shoulder or neck depressing shoulder, or fulls
stretching head away from shoulder.
c. Falls when the arm catches, suspending the person at least
momentarily, or where arm is twisted.
d. Being lifted by the arm as over a pulley, or dragged forci
bly by the arm as in case of children jerked by parents
leading them by the hand.
e. Accompanying dislocations or the reduction of dislocations.
f. Prolonged holding of arm in abduction and external rota
tion, as in operation.
g. Slipping while carrying a weight on shoulder. h. Sudden movements, as in effort made in trying to lift weights.
2. Pressure.
a. Dislocation, where shoulder is out for a long time. b. Exuberant callus, especially of the clavicle.
c. Saturday night paralysis, usually radial, terminal.
d. Crutch paralysis, terminal.
e. New growth, involving roots, trunks or terminal branches,
secondarily, either from bony, cartilaginous or soft tissue
pressure. 1. Benign. 2. Malignant.
f. Adventitious rib or bands.
g. Strait-jacket; several cases have been reported, but al
ways where the patient freed the arm so as to cause con
striction.
h. Following aneurism of the subclavian or axillary artery. i. Esmarch bandage or tourniquet. j. Degenerative bone lesions of the cervical spine, especially
tuberculosis, causing pressure on roots. k. Fractures; especially of vertebras, by direct pressure.
3. Direct Injuries.
a. Cuts or wounds.
b. Fractures or dislocations causing direct injury.
c. Injection of the plexus by local anaesthetics.
d. Electric shock.
4. Toxic.
a. Following serum injections.
b. Infectious diseases, especially pneumonia.
c. Following anaesthesia, chloroform especially. (These are
hard to separate from possible trauma from mal-position
during the anaesthesia, but several cases have been reported
where no mal-position could have occurred.)
d. Poisons—as lead—usually peripheral neuritis.
5. Spinal Cord Lesions
a. Infection.
b. Degenerative processes.
c. Tumors.
d. Direct injuries to the cord itself. e. Hemorrhage within vertebral canal.
6. Psychic Paralysis. (Hysteria.)
7. Central.
Monoplegia. Rare; never complete; spastic, not flaccid.
This list covers most of the causes of injury, but cannot indicate the relative frequency in which they occur; no such statistics have ever been collected. As a matter of fact, in a very large majority the injury is of the traction type. In a smaller number it may be of the pressure type. The lesions caused by the remaining five types are either too rare or too obvious to be discussed here. Most of the common injuries have to do with temporary, partial or complete displacement of the head of the humerus. The plexus may be injured by the same force acting concomitantly directly on the plexus, or by the prying effect of the displaced head on the cords themselves. If the head of the humerus remains out of position for some time, direct pressure on the plexus itself may be a factor. As indicated in the diagram below, brachial plexus injuries may be classified for purposes of study in several ways besides the etio-logic grouping given above.
.jpg)
FIGURE 63. DIAGRAM OF NEUROVASCULAR CORD
The primary division into supra- and infra-clavicular lesions is important, not only because in the literature of the subject one finds endless discussion as to which group is the more common, but because when surgical exploration has been decided upon, one must choose between the upper or lower field for the incision. The secondary divisions obviously cannot be made strictly in subdivisions of the primary division, for a small part of the trunk lies above, and a large part below the clavicle. All root lesions are necessarily above the clavicle, and all lesions of the great terminal branches, including the axillary, are below the clavicle. However, some of the smaller but highly important upper terminal branches, usually spoken of as "the root collaterals," such as the dorsalis scapulae, suprascapular, phrenic and long thoracic, are above the clavicle since they arise from the roots, or from the fasciculi not far from the roots.
In the text which follows, we shall frequently allude to that part of the plexus between the junction of the roots and the origins of the great terminal branches as the "trunk." This trunk when dissected is the "plexiform part." Since in most of its extent the "plexi-form part" forms a compact bundle about the axillary artery, we also speak of it as the "neurovascular cord" or "integrated cord." This fascia-bound structure is a very real anatomic entity, although somewhat vague in all its limits, since each structure that enters or leaves it contributes or carries away accompanying strands of fascia. It is a single cord closely integrated by dense fascial investment from just beyond the interscalene segments to well below the shoulder, a single cord which flares out at the base into five roots of varying sizes, and, far below the apex of the axilla, flares out again into its terminal branches.
Root paralyses. The Erb-Duchenne, or upper type of brachial plexus palsy, is the most common form of paralysis from root injury. It was described in detail with only minor differences by both Duchenne (1872) and Erb (1874). It is accepted as a paralysis of the supra- and infra-spinatus, the deltoid, the biceps, the brachialis and the brachioradialis. If the lesion is far back on the roots, we are told that the paralysis usually includes the levator anguli scapula, the rhomboids, and sometimes the serratus anterior and the portion of the diaphragm supplied by the phrenic nerve. If these muscles are paralyzed it clinches the root diagnosis. If they are not, it does not exclude it, for anomalies occasionally exist. Accurate statements as to the condition of the muscles are too seldom included in most of the reports of examinations of cases of brachial paralysis. Many cases of deltoid, biceps, brachialis and coraco-brachialis paralysis have been reported as Erb-Duchenne, but inclusion of the supra- and infra-spinatus and the brachioradialis is necessary for a diagnosis of this type. The coraco-brachialis, the supinator, and, as Harris pointed out years ago, the extensor carpi radialis longus and brevis are sometimes also included in this type, as will be explained later. The pronator teres may also be involved, for it frequently is supplied from the 6th cervical nerve. When the posterior part of the deltoid, which is also probably supplied by the 6C, and the pronator teres are involved, it raises the question of inclusion of the 6th at least. Probably the innervation of the pronator teres may sometimes come from the 7C. That of the coraco-brachialis and extensor carpi radialis longus and brevis may also more often come from the 7C than from the 6C.
Harris called attention to the fact that the inclusion of the 6C in a root lesion usually added nothing to the extent of the paralysis caused by a 5C involvement, and Sherren and other observers have agreed with him. So that the 6C is to be regarded as a sort of makeshift root, its inclusion adding little to the severity of the paralysis.
The clinical term "Erb-Duchenne paralysis" has come to be used very loosely. It no longer defines, as it should, a root paralysis of the 5C and 6C, but is extended to include cases which involve the 7C. The involvement of the 7C should place the case in the complex type. The term is also applied thoughtlessly to peripheral lesions of the axillary nerve, and even to cases of lead palsy in which the axillary is involved. Moreover, the term Aran-Duchenne paralysis is sometimes confused with it, and is erroneously used. This term indicates an entirely different pathologic condition, due to a degenerative lesion of the anterior column cells. It usually first affects the small muscles of the hand and is slowly progressive, and finally at least is bilateral. The careless use of these terms, without definite statements as to exactly which muscles are paralyzed in each reported case, renders many articles worthless for purposes of detailed study.
It is usually agreed that there is remarkably little sensory disturbance with the Erb-Duchenne type, and that this is confined to the axillary distribution on the external or postero-external surface of the shoulder; but all observers are by no means in accord with this, especially Rendu. Andre Thomas's two cases, of cut 5C and 6C, and of cut 6C root alone, both showed a well-marked sensory disturbance, not confined to the axillary distribution.
The lower or Dejerine-Klwnpke type, due always to an involvement of the 8C and ID roots, is a combined paralysis of the flexors and extensors of the forearm with integrity of the brachioradialis, supinator, pronator teres and the extensor carpi radialis longus and brevis. The intrinsic hand muscles are paralyzed and the upper arm extensors (triceps) are partially involved. In this type sensory disturbances are much more profound. Trophic and vasomotor symptoms are sometimes pronounced, although some observers believe that in a pure brachial plexus lesion, vasomotor and trophic symptoms are not pronounced. As few such injuries are pure, this is a fine distinction. Vasomotor and trophic fibers come via the autonomic to their somatic nerve distribution.
The syndrome of Poirier, or as the French call it today, the syndrome of Claude Bernard-Horner, is present when the ID is involved far back on the roots, and is caused by involvement of the rami com-municantes which pass to the stellate ganglion. It is shown by miosis, enophthalmos and ptosis on the side of the lesion, with preservation of the light reflex and accommodation; there is normal tension or slight hypotension and normal vision, but abolition of dilatation of pupil to cocaine.
Miss Klumpke's* contribution to the subject of brachial plexus injuries has given her name to this lower root type. Her report included three cases of her own which she followed in the Clinics of Vulpian and Lucas De Championiere, but only one was of this lower type. None of her own cases was proven by operation. The rest of her eighteen cases had been reported by other men and included the case of Flaubert. Her real contribution was her experimental work on animals, by which she proved that the syndrome of Poirier or Claude Bernard-Horner followed a section of the first dorsal root back of the ramus communicans to the stellate ganglion, and that it occurred only after section of the ID or of the ramus itself.
*Miss Augusta Klumpke (1859-1927) was the eldest of four brilliant American sisters who were born in California and later educated in Switzerland. She studied medicine in Paris and achieved the distinction of being the first woman interne to serve in the Paris hospitals. In 1885, soon after her graduation, she published an article on paralyses due to injuries of the lower roots of the brachial plexus, a type which has since been designated either as "Klumpke paralysis," or as "Dejerine-Klumpke paralysis." This confusion has arisen because five years after the publication of this paper she married Professor D6jerine, a neurologist and also a pupil of Vulpian's. They were later joint authors of numerous books and papers considered among the foremost landmarks in the progress of modern neurology. The three younger sisters also became distinguished in their chosen fields, of astronomy, music, and painting. The youngest, Miss Anna Klumpke, is widely known as an artist and as the friend and biographer of Rosa Bonheur.—E. A. C.
An intermediate type of brachial plexus paralysis, due to involvement of the 7C root alone, is practically non-existent, except as an accompaniment of either the Erb-Duchenne or the Dejerine-Klumpke types, when it would be classified as " Complex." The pure 7C paralysis would be a partial paralysis of the extensors of the arm, forearm and wrist, including the abductor longus pollicis and the extensors of the thumb. As the coraco-brachialis and extensor carpi radialis longus and brevis and the pronator teres are supplied by the 7C at times, these would therefore sometimes be included in the paralysis, but as these last come also at times from the higher roots, they might not be involved. A knowledge of the condition of the root and trunk collaterals from the 7C and the intermediate fasciculus, would not be of as great help in diagnosis as in either of the other types. The lower part of the serratus anterior might show a paresis, but as it receives branches from the 5C and 6C, it would not be entirely paralyzed. The same applies to the subscapularis and the latissimus dorsi, which, while receiving fibers from the 7C, also receives at least as great an innervation from other roots.
Complex types. As a complication of the upper type, the inclusion of the 7C adds to the usual group of muscles the following: partial paralysis of the extensors of the arm, forearm and wrist, including the extensors of the thumb; a more profound involvement of the trunk collaterals to the latissimus dorsi and teres major; the entire paralysis of the subscapularis, the coraco-brachialis, and the epicondylar muscles.
As an accompaniment of the Dejerine-Klumpke type, the inclusion of 7C is indicated by the addition of absolute paralysis of the extensors of arm, forearm and thumb to the other symptoms of a lower type paralysis. In this type the subscapularis paralysis is never entire, but the latissimus dorsi is likely to be entirely paralyzed. The pectorals are seldom entirely paralyzed except in a complete lesion of all roots. The upper part of the pectoralis major, i.e., the clavicular portion, is included in an upper type, and the lower part is involved in a lower type together with the pectoralis minor.
The complete type. In very rare cases where the arm has almost been pulled off, all, or nearly all, of the roots of the plexus may be injured.
In the period from 1870 to 1890, there was much discussion, particularly among the French, as to the exact location of root injuries, i.e., whether the rupture occurred within the spinal canal and involved the cord (avulsion de la moelle epiniere), or in the bony gutters formed by the transverse processes, or between the point of exit from these gutters and the point where the roots join to form the fasciculi. The term "radiculo-medullaire" was also used in an almost synonymous sense with avulsion. It is probable that today the French neurologists may have dropped these terms or attached other shades of meaning to them than those which we have interpreted. However, we must present these terms because they have been so much used, although the writer is satisfied from his own observations on the cadaver that nearly all injuries must occur entirely outside of even the bony gutters, because careful dissection shows that the roots are always snubbed at the transverse processes, i.e., attached to them by fascial connections. The reasons for believing that this snubbing will usually prevent injury to the roots within the canal, or even within the bony gutters, will be given later.
Some authors (e.g., Shallow) have found at operation cysts containing cerebrospinal fluid close to the transverse processes, and have concluded that this was evidence of an evulsed root. This does not seem to me sound, because tubular processes from the dura not infrequently extend beyond the transverse processes and would be ruptured with the snubbing. (Fig. 63.)
Gross anatomy of the intact plexus. Before we take up in detail the study of the distribution of the nerves to the various muscles of the arm, it is necessary to consider the plexus as a gross unit, for we must always remember that in the body it has not been dissected and does not lie in the form of a diagram.
In the last sixteen particularly careful observations I found that each root of the brachial plexus was held firmly at the transverse processes and in the gutters of bone by invaginations of the prevertebral fascia., In the words of the mechanical engineer, each root is snubbed at the transverse processes. There it is firmly fixed. If it were not, and there was nothing to take the ordinary strain away from the spinal cord itself, a man might be paralyzed at any time by a strong pull upon either the arm or shoulder.
Below the clavicle, the cords of the plexus are firmly bound together and also to the surrounding structures, including the clavicle and the coracoid, by layers of the clavo-pectoral fascia. The three main cords join the subclavian artery as soon as it appears above the first rib, and remain integral with it in its course through the axilla. The clavo-pectoral fascia comes down from the back of the fascia which surrounds the subclavius muscle, forming the costo-coracoid membrane. This membrane goes to the coracoid and joins the axillary fascia below. The clavo-pectoral fascia leaves the back of the costocoracoid membrane, passes between and invests each branch of the brachial plexus, surrounds the axillary artery and is continuous above with the prevertebral and below with the deep fascia over the first rib. Therefore, the integrated neurovascular cord is snubbed again, as well as at the transverse processes, by these fascial investments between the clavicle, the coracoid and the first rib; that is, in the apex of the axilla.
I should like to acce"nt the facts in the preceding paragraphs because I believe that these points of attachment help to explain the different types of lesions resulting from a blow or stress above the clavicle, and also those resulting from stresses which come through the arm from below, either as straight tension, or as lateral stresses resulting from dislocation. I have been interested in the mechanics of the shoulder for many years, and have studied on the cadaver the probable relation of the plexus to the displaced bones in cases of fracture and of dislocation, and the conclusion has been reached that the explanations found in the literature of the mechanism of the involvement of the plexus in these injuries are not adequate.
I shall discuss the theories which have been offered to explain the mechanics of the more common lesions of the plexus from trauma, and then offer one which I believe shows why the plexus is either injured at its roots beyond their exit from the spine and before they join with others to form the plexus, or in its terminal branches, and never (except by cuts or wounds) in the plexiform part, which, nevertheless, is usually involved secondarily by hemorrhage and exudate between the nerve bundles.
Most observers, up to the time of Horsley, believed in a local injury to the brachial plexus, both in birth and adult cases. Erb believed that the injury was due to clavicular compression, but this idea was gradually destroyed by Gerdy, Fieux, and Horsley. The idea of root lesions originated with Secretan, and thereafter there was a division of these cases into root, trunk and terminal lesions.
To Gerdy is given credit by the French of the traction theory, that is, straight pull as the cause of these paralyses, although Malgaigne knew it long before this, for he had paralyzed two cases himself in reducing dislocations by a direct pull of 200 to 250 kilos (more than 500 pounds). Flaubert must have known it, since he had thus caused paralysis not only in his celebrated case of 1827, but also in two others, by direct traction. Various experiments have been made, and a great amount of time has been spent on the mechanics of these lesions. The case of Flaubert was the starting point of the avulsion theory, that is, the separating or pulling out of the roots from the spinal marrow itself. This, we contend, is rare except in very violent injuries.
To Horsley, in England, is credited the idea that the lesions are caused by injuries which tend to spread the head and shoulder apart and thus to stretch the plexus. Today this is generally accepted as the most likely theory of production. Horsley's experiments are not given in detail, but in the Practitioner, of London, he said that by dropping cadavers on head and shoulder, he had been able to break the plexus.
Duval and Guillain, in 1898, made an extensive study of the plexus anatomically, carefully estimating the different angles formed by the individual cords from their origin at the spinal marrow to their emergence under the transverse processes of the vertebrae and across the neck to the arm. They assumed a transmission of stress by tension to the roots, which, because of their angulation, was more or less expended as ecrassurage (crushing), at the points where the roots angle around the transverse processes. They held that this action was enhanced on the lower roots by elevation of the arm, and especially on the first dorsal root as it wound around the neck of the first rib. They believed also that the force was transmitted far back even to the spinal marrow in most cases.
In dislocation they believed that traction fell on the roots at the same time that it caused the dislocation, rather than that lateral stress was caused by the dislocating head. Most of the French and German profession accepted this explanation, and the idea that a supraclavicular, even radiculo-medullary lesion took place in most of these brachial plexus injuries became more and more engrafted in the minds of surgeons and neurologists.
It remained for Delbert and Cauchoix to point out in a very wonderful paper in the Rev. de Chir., in 1910, that many of these supposedly supraclavicular lesions that had been diagnosed as radiculo-medullary, root or trunk lesions were in reality lesions of the axillary portion of the plexus; that is, terminal, and especially so when they accompanied dislocation of the shoulder. They reported three operated cases of their own, and the rest were interpretations of cases previously reported by others; but only a few were checked cases. They believed that the injuries were high up, i.e., root lesions, or low down and terminal, but not of the plexiform part. In this last conclusion we agree. They studied thirty-six cases, all dislocations; and they believed, as did Duval and Guillain, that the nerve lesions were due to the same stresses which caused the dislocation, rather than to lateral stress from the displaced head of the humerus. Their paper never has received the attention in America to which it is entitled. It is probably true today, when one speaks of a brachial plexus paralysis, that the majority of American surgeons visualize a lesion of the nerves of the plexus high up above the clavicle, either trunk or root or even radiculo-medullary, and give little thought to the possibility of infraclavicular peripheral injuries, especially to those of the axillary nerve.
There has been, we believe, a misconception in the minds of the profession regarding the frequency of brachial plexus rupture. True rupture, with complete separation of the torn ends, is a rare lesion either above or below the clavicle, whether of root or terminal branch, as compared to cases of injury without rupture. The cases of proved rupture, although few, are extremely important, both as to their mode of production and as to the exact point of the plexus which has suffered the separation, because from a study of these proven cases, it is easier to understand where the acme of stress is most likely to fall, in those less severe and much more common cases where paralysis supervenes without actual loss of continuity in any part of the plexus.
It has been said by various authors that Bowlby was able to collect nineteen cases of frankly supraclavicular rupture of the plexus, that Bristow added three more proven cases, and that Frazier and Skillern were able to collect records of twenty-one cases of actual supraclavicular rupture. Examination of all these original papers shows that Bowlby reported nineteen cases of brachial plexus paralysis, but only three of them were checked, namely, one case of his own, where operation was in the axilla and nothing was found; the case of Banks of actual proven rupture, which had already been reported; and the old case of Flaubert of actual avulsion, which has been reported so many times. Bristow reported one case of his own of actual rupture, and another case of actual rupture which had already been reported by Hartley. His third case was by no means proven; he attributed it to Senn because Senn had told him that he (Senn) had had a case. No details of this, whether proven or not, were included. Frazier and Skillern reported only one case of their own of actual rupture, and the celebrated case also reported by Mills; their others were cases from literature without detail, and again included the case of Flaubert. Frazier simply said that in the literature he had found records of twenty-one cases with proven rupture of one or more roots, without skeletal injury. It may, therefore, be understood upon how little foundation theories as to the causation of brachial plexus ruptures now rest.
DR. STEVENS' THEORY OV MECHANISM OF PRODUCTION OF BRACHIAL PLEXUS INJURIES
A cord to be broken in tension, whether by a blow on its side transmitting the stress to both ends, or by direct pull, must be held firmly at the ends or there will be no tension. The brachial plexus is so held by the fascia, as we have shown in our dissections and by the description already given.
All cases of plexus injury of the type under discussion are due to tension, that is, traction. It makes no difference as to the basic mechanical stress whether a man slips carrying a heavy load; whether he is struck by a blow, depressing his shoulder; whether there is straight traction on the arm; whether his head is forced away from his shoulder; whether his face is rotated away from or toward the side undergoing stress; whether the arm is pulled in abduction and in external rotation; whether or not his arm is raised, lowered, supi-nated or pronated; if the stress is reflected on the cords of the plexus, it is tension. However, the different varieties of stress and the relative position of the ^rm and head at the time of stress, make tremendous differences in the kinds of lesion suffered, in the locality of the lesions and in prognosis. The nature, location, and seriousness of the injury, I believe, depend on whether or not the stress is received from above or is transmitted from below; whether or not the arm is above or below horizontal, and whether or not externally or internally rotated. These factors, together with velocity and magnitude of stress, determine, in most cases, the severity and the locality of the injury. Nevertheless, in all cases the stresses are of the same nature.
Consider the cords of the brachial plexus as a traction apparatus with its normal axis as a mechanical appliance on the 7C vertebra, with the arm at the horizontal, i.e., a single cord with five separate points of attachment firmly snubbed at the transverse processes.
When tension is applied to this structure (the integrated cord), it falls on the offset roots. Any mechanical engineer will tell you that an arrangement of this kind will rarely transmit stress through five cords equally. If the force of the pull could fall exactly through the neutral axis at the exact center, and at an exact right angle to the base or plane of the structure to be lifted, the size of the cords being the same, it might be possible to lift a weight evenly, but he will also tell you that stress always tends to travel in straight lines, and depending on the position of the application of stress, the acme will usually fall to one side or the other of the neutral axis of such a structure.
.jpg)
A suspension apparatus is governed by much the same laws as a traction apparatus. In engineering a three-point suspension is more reliable than a suspension from a greater number of points. Perhaps this is the reason why three roots are injured in so many cases of brachial plexus paralysis, for either the two upper roots or the two lower ones may combine with the median root.
A traction apparatus must have a neutral axis and a hne of resistance, and when the force of traction falls through this neutral center or axis, the traction is equally borne by all parts of the apparatus. Even a slight deviation from this neutral axis makes an offset pull to one side or the other, and in a structure of this kind, if the line of tension falls outside the neutral axis, as represented by the line of resistance, the entire force is transferred from that neutral axis; all tension is released on the cords on the other side, and a new neutral axis is instantly formed about the components which are now bearing the stress, to conform to the new line of resistance. All other components are out of the structure; they are lax and their influence is nil.
A pulley inserted as part of a traction apparatus is not placed so as to change the degree of pull on the structure to be lifted or moved. It is placed there in order to change the direction of the application of the force in order to make it more convenient or effectual, i.e., to keep the neutral axis in the desired direction. The pulley must be so placed that a line from the pulley to the center of the structure to be raised or moved, falls through the neutral axis and the line of resistance. If this is not so, the force applied falls to one or the other side of the axis and the entire force of the pull may, therefore, fall to one side. If you elevate the pulley, the lines of tension and resistance will come below the neutral axis as it existed at first, and the acme of stress will be below. If you lower the pulley, the acme of stress will be above. Since the scapula is movable and the integrated cord passes under the arch formed by the coracoid and the pectoralis minor, a condition similar to a movable pulley exists in the shoulder.
There is no real pulley, but the cords of the plexus are held in this arch and, as the arm is raised and the clavicle and the coracoid rise, the latter acts much like a pulley, for it changes the direction of any force applied distal to it. In raising the arm, when the coracoid rises above the horizontal, the acme of stress would come on the lower roots. (Fig. 64c.) Lowering the arm lowers the coracoid, and the acme of stress is on the upper roots. At a horizontal, the neutral axis is near the 7C vertebra, and all roots might be stressed evenly, because the neutral axis, the line of tension and the line of resistance correspond. As a matter of fact, when the continuity of the bones is intact, the range of the coracoid is such that like a self-adjusting pulley it maintains the direction of pull very nearly in the neutral axis, as the arm moves.
As an exaggerated example of how the coracoid can change the direction of stress, suppose a man caught in a machine in such a manner that, while the arm is abducted in the scarecrow position, two parts of the machine travel in opposite directions, one pressing the elbow upward and the other part pressing the shoulder downward. The coracoid will be depressed, hooked over the taut plexus, and the force transmitted to the upper roots. The stress would be downward on the upper roots, even if the pressure above the shoulder remained fixed and only the elbow continued to be forced upward.
With the arm at the side and pulled downward, the pulley is not the coracoid, but the place where the plexus comes over the first rib anteriorly. This slight change of direction of the force would relieve, to some extent, the strain on the upper roots in a downward pull* Combined with this would be help from the clavo-pectoral fascia.
A breaking strain expended on the brachial plexus from above, as from a blow on the shoulder, or the stress suffered when one slips while carrying a weight, usually should cause a lesion of the 5C root. Five cords divided will not stand the strain as well as when they are combined in one.
The apparatus will break at the weakest point, i.e., at one of the roots between the point where it is snubbed on the transverse process and the junction of that root with others. It breaks there, or it does not break at all in supraclavicular stresses. If it does not break, nevertheless the acme of stress is at the same point.
In this case of a blow from above on the neck or shoulder, or a slip while carrying a weight on the shoulder, "the integrated cord is stretched, and the stress in both <sases is transmitted to the points of firm attachment of the cord at both ends. Here is impact, and impact is infinitely greater than static load. A man carrying one hundred pounds on his shoulder slips or makes a false step, and falls even four to six inches. Instantly his static load, which he could carry with ease, becomes an impact trauma. The mechanical stress suffered here is exactly the same as it would be if he were struck on the shoulder by a hundred pound hammer falling through four to six inches and depressing the clavicle and the coracoid. The brachial plexus is instantly stretched between its two firm points of attachment, which are, as we have shown, at the transverse processes above, and at the clavo-pectoral fascial snubbing below, in the upper axilla. Again, the stress in tension is exactly the same as if the cords themselves received a side blow. Impact, as the mechanical engineer will tell you, so increases a stress over static load as to be almost unbelievable. (See Merriman, Mechanics of Motion.)
When surgeons contend that rupture of the roots would be impossible in the ordinary trauma, or in that due to dislocation, they fail to take into account the manner in which mechanical stresses may be magnified at the point of final application when they fall on structures of limited area. The reason that the roots do not always break, is that the stress does not fall on these limited structures alone in many cases. It is disseminated. In both cases cited above, the stress is transmitted to both points of attachment. One half is referred back to the roots, the other half falls on the place below, where the cords are held firmly by the clavo-pectoral fascia. So that sometimes, even in this type, we have an accompanying rupture or injury to the artery, because the fascial snubbing surrounding the cords gives way and the vessel is torn. Injury to the artery probably happens less often in case of blows from above than when the stress comes through the arm from below as pure tension, because in the latter case, the entire force of the pull is not divided. It falls first on the clavo-pectoral fascial snubbing, and is then transmitted back to the pulley at the first rib and the roots, but not until the fascial snubbing in the axilla has been injured. It is quite possible that we might have traumatic aneurism without rupture of the roots, because the stress might be disseminated after the fascia and the vessels have been injured, and then be too weak to break the roots.
In a very careful review of the literature the writer has been unable to find a single case of rupture in the plexiform part of the plexus, i.e., in that part which has been alluded to as the neurovascular cord, although the artery itself may be torn. Even proved injuries of this portion of the plexus from bullets or cuts are rare, but we are speaking now of rupture from trauma without a penetrating wound. In reading the accounts of operations, on the other hand, one usually finds such statements as "the plexus seemed a mass of scar tissue," "the cords were welded together in an inflammatory mass," "on account of the scar tissue, nothing could be made out as to the exact location of the injury," etc., etc. Yet many such cases have recovered in whole or in part, indicating that no real rupture had occurred in the nerve fibers, and that the gross appearances were due to ecchymoses, exudate, or scar amongst the fascial envelopes and fibrous septa in the nerve trunks. In this region, as in others, intensive anatomic study of the mechanics of the structures reveals marvellous examples of architectural and mechanical designs, e.g., the integrated cord when dissected is "plexiform," after the fashion of a complex design of parallelograms of forces. This is an admirable arrangement to disseminate stresses, for if the cord were pulled at both ends, before rupturing the longitudinal strands, the force must break the little lateral bands of tissue which we cut when we dissect the plexus. It is probable that many little local hemorrhages, about, amongst, between, and within the individual trunks, cause the appearances so frequently described. Subsequent exudate and scar tissue complicate the picture, and choke the nerve fibers, usually temporarily only.
I believe the explanation of these injuries to the plexus is this simple mechanical one; in any case it has nothing whatever to do with the idea of ecrassurage against either rib or transverse process. The stress will not be "radiculo-medullaire," except in very rare cases of sudden, violent injury, because to be so, the mechanical apparatus would have to break back of the snubbing, and that is contrary to the laws of mechanics. The snubbing is stronger than any individual root, but it is not stronger than the entire integrated cord.
If the stress comes from below through tension on the arm, there must be some separation of the bony framework at the shoulder, before stress can be transmitted to the soft tissues. For instance, the clavicle might be broken, or the humeral head might be pulled away from the glenoid cavity, or when dislocated, pried against the plexus. In postoperative paralysis in breast cases, the muscles are relaxed and the plexus assumes the stress. In cases of fracture of the clavicle when paralysis is a complication, we should think first of a root lesion, and only secondly of injury to the cords from actual contact with fragments.
Estimate of Comparative Strain on Integrated Cord and Root.
Some idea of the strain to which a root is subjected in one of these injuries, in comparison to that sustained by the integrated cord, may be obtained by reference to Fig. 64.
If the pull remains the same the stress per square inch becomes rapidly greater the smaller the cord. Engineers use the formula
Pull / Pi R (squared) = stress per squar inch
By using this formula and assuming the integrated cord comprising the artery, fascia and nerve trunks to be one-half inch in diameter, we find that a pull of one hundred pounds would exert over five hundred pounds stress per square inch on the cord as a whole. If all the other components were removed and this stress fell on one nerve root one-tenth of an inch in diameter, this root would have to receive over 12,000 pounds of stress per square inch of its cross section, which, of course, would rupture it. If the stress fell on two roots, it would be divided. In order to determine the comparative stress on these two roots, we use the parallelogram of force of the mechanical engineer, Fig. B. Therefore, if it is a breaking stress, the roots never break together; one gives, and then the entire stress falls on the next, etc., until dissemination of force stops the process. With stresses as above, why do these cords not always break? Simply because these stresses do not often fall on the cords in this way. Other structures, bones, ligaments, muscles, tendons, fascia, etc., receive some stress, but the bulk of the stress may thus fall on one root or two roots, and sometimes does.
Considerations such as these make us wonder at the remarkable arrangements which nature has supplied to prevent stress falling on any one root of the plexus. When a mother drags her child across the street by one hand, there are many anatomic structures which protect the plexus. The bones and ligaments form a chain which takes most of the stress. Should there be a loss of continuity in this chain, the coracoid process acts as a pulley to distribute the stress in the neutral axis of all the roots. Even when the stress arrives at the roots, the two lower ones join together and the two upper roots join together before they unite with the middle root; thus, the upper cord and the lower cord each form a two-point suspension, and the middle root is somewhat protected. When the two points formed by the upper and lower pairs unite with the 7th or middle root, we have a three-point suspension. These three-point suspensions then form the plexus, which is so arranged that each main cord and nerve is attached to its neighbors by fascial binding, uniting them into a trunk capable of sustaining much stress. Even then, when they pull apart, the fascial bindings between the cords must be torn before any individual cord may be torn. However, there are occasions when, owing to rupture in the continuity of the supporting structures, all stress will be thrown on either the uppermost or lowest root. Even then there remains the snubbing of the fibrous envelope of the nerves to the transverse processes to protect the spinal portions of the roots. Fainting, anaesthesia, or other forms of unconsciousness which relax the muscles remove a very important factor in protection.
The Theory Applied to Ruptures of the Terminal Branches.
Let us now consider the stresses which often result in terminal branch lesions. Imagine an arm in abduction and external rotation subjected to still greater backward stress,* This is the position of dislocation, and lateral pressure on the taut plexus takes the place of pure tension on the whole arm structure. By this position of abduction and external rotation you have separated the terminal branches of your cord as much as possible, and if lateral pressure is applied, your apparatus is no longer a single cord with five lesser points of attachment where it is joined to the transverse processes; it now has six or eight separate smaller cords below, any one of which may have to take the major stress. In other words, you have added other factors to your mechanics. Offset may now fall, not alone on the roots, but at the other end of your apparatus. If it falls on any terminal branch that is smaller or weaker than any part of the integrated cord or roots above, it will break that terminal branch below its point of insertion into the integrated plexiform part. If, however, the main stress should fall through the radial nerve, which is greater in strength and size than most of the roots, it would probably be transmitted back to the roots as the weaker points. I have found in many dissections that the posterior or intermediate cord is as high in the neck as the lateral fasciculus. Force applied to the radial would be transmitted through the integrated cord back to the 5C and 6C to a greater degree than to the 7C, from which its motor portion arises originally. The weaker points are below and at the roots. This is why there have been ruptures reported of the musculocutaneous nerve, of the median heads and of the ulnar, at their origins in the axilla. We have many reports of injury involving each of these nerves in the axilla (forty-four operated cases), but there is no proven case of absolute rupture of the radial alone. Why? Because it is stronger than the clavo-pectoral fascia which binds it, and while it is weaker than the plexiform part of the plexus, and would break before that, it is stronger than the roots themselves on which individually, because of offset, the stress may also fall.
When we speak of a root, or a cord, or a nerve, as stronger or weaker, we mean that cord or nerve bound with connective tissue. No root or cord breaks until after its sheath has given way. No nerve can be stressed -until its surrounding fascia gives.
The fact that fifteen cases of subclavian or axillary aneurism have been reported in conjunction with 135 injuries to the plexus, suggests that the clavo-pectoral fascia surrounding the integrated cord is usually stressed and often actually torn. In most of these cases there was only one incision, either a supra- or an infra-clavicular one, so that the conjunction of high and low lesions is probably greater than indicated in these figures. If in each case both incisions had been made, a still greater coincidence of fascial and arterial injury might have been shown.
*In this position the terminal branches tend to separate from one another, and in the opposite position (internal rotation with the arm at the side) to continue their course almost side by side.—E. A. C.
Application of These Principles to Axillary (Circumflex) Nerve Injuries.
In dislocation of the head of the humerus, we have the cause of the greater number of axillary nerve paralyses. We have at times in addition injury to each of the other nerves in the axilla, and through the radial, for the reasons stated above, we may also have as a result of the stress of the rotating head, injury transmitted back to the roots. The axillary nerve is most often injured because in dislocation it is tensed across the head in the erect phase when the arm is elevated and externally rotated. The axillary is the one nerve which at this point has already separated, and is an individual cord. It is closely applied to the anterior surface of the subscapularis muscle, and is carried with the head when it turns out of the lower part of the glenoid. Since the subscapularis tendon is anterior, and firmly attached to the lesser tuberosity, this nerve must be more or less stretched in every case of anterior dislocation. The axillary is particularly vulnerable because it is firmly attached above to the main cord, and is snubbed below, where it passes back to wind around the neck of the humerus. Therefore, it is a short length of nerve subjected to a side stress, which is again nothing more than tension transmitted to both ends. The wonder is that it is not always paralyzed in cases of dislocation.
Confined solely to the axillary nerve would the stress be transmitted back to the roots? It would not, for the axillary is weaker than the plexiform part of the plexus, and it is weaker than any root. The axillary is stressed most often alone, not enough to rupture it, but enough to paralyze the deltoid. If it breaks, it will break between the place where it leaves the intermediate fasciculus and the place where it passes between the subscapularis and the teres major muscles, and nowhere else, because this is the weakest point. This accounts for the fact that simple deltoid paralysis is far the most common nerve lesion complicating dislocation.*
*In such cases the patient might still be able to elevate the arm with the supraspinatus.—E. A. C.
In our series from the literature, there were only three cases of actual rupture of the axillary nerve, aside from many cases of injury where the exact pathology was not determined by the operation. In addition, Weir-Mitchell reported nine cases of ruptured axillary, years ago, but they were not checked by operation.
The cases of musculocutaneous paralysis (aside from rupture), which have been reported, may be, and sometimes are, due to the mechanics already described. We believe they may be caused also by the pressure of a dislocated head which has been left out for a long time, although the nerve may be stressed by the rotating head in dislocation, especially in the first phase, exactly as all the others may be stressed. The idea that these nerves slide up and slip over the head of the rotating bone with any degree of facility is absurd. The only way they slip over the head is because the head of the bone is rotated under them, in spite of tension, and in spite of their being plastered in place by the tremendous contractions of surrounding muscles which are resisting injury. This nerve is also snubbed at its junction with the integrated cord above, and it is snubbed where it passes through the layers of fascia both internally to the biceps and beneath it, and where it usually passes through the coraco-brachialis muscle. Like the axillary it is a short cord which is being tensed by a side stress. It may be injured in this way or even ruptured, but we believe that many times as the dislocated arm falls back to the side, the musculocutaneous nerve, in this new position, is unable to free itself, and remains tensed over the dislocated head, until reduction frees it.
A case of subcoracoid dislocation of the right shoulder, caused by a fall, was observed by the writer in 1929. It was three hours before the dislocation was reduced, during which time the patient swung his arm, because he said that although it hurt him to do so, it felt better when he did it. He had a sensation of pins and needles during this time in arm and forearm. Reduction was not followed by abduction treatment, but the arm was supported by a swathe and sling. When he returned four days later, paralysis of the biceps, brachialis and coraco-brachialis was found. Two weeks later the reaction of degeneration was present in these muscles. No others were paralyzed. Epicritic loss was greater than protopathic in the domain of the musculocutaneous nerve. The absence of brachioradialis and supinator brevis paralysis, the absence of supraspinatus, infraspinatus, deltoid or teres minor paralysis, the presence of coraco-brachialis paralysis and the fact that paralysis did not occur at once, make it probable that this was an injury of the nerve in its axillary portion. It is best explained by compression from infiltrate which came as the result of long-continued pressure. First voluntary motion appeared at the end of eight weeks, and recovery was very rapid thereafter.
Although they are very common, very few cases of isolated deltoid paralyses, or combined paralyses of the deltoid, biceps and brachialis, appear in the literature, because many of them are mild and recover in a few months. Nevertheless, I believe that axillary injuries of the brachial plexus are much more numerous than supraclavicular injuries, and also, in the main, less serious. In this instance, ordinary practical experience is of more value than recorded literature. Lesions of the plexus caused by, or at the time of, dislocation usually soon get well; cases in which recovery is prolonged or eventually imperfect are those in which the shoulder as a mass has been suddenly depressed. Thus I believe that with a knowledge of the actual trauma which was sustained, it is possible to arrive at a better conclusion as to prognosis than it is from the clinical symptoms alone.
Avulsion of the nerve roots from the spinal cord ("radiculo-medul-laire") must be very rare. There are only four cases of proven avulsion which I have been able to find in the literature and I shall speak of these later. In these four cases at least there can be no doubt of the lesion. How can we explain the mechanics of the avulsion cases, if, as we have said, the anatomical arrangements predispose toward more peripheral injuries? The simplest explanation is this: The mechanical engineer will tell you that in the face of tremendous stress, where velocity of stress is great, all rules governing stresses and strains fail. In the face of a tremendous stress with velocity, the snubbing of the roots at the transverse processes would give way and the stress be then applied to the nerve fibers within the vertebral canal. It is significant in these four cases that in not one was the 5C broken. It is evident in all that the stress fell through the 7C and the 8C, which are certainly the largest of the roots. The cause in each case was a direct pull in nearly the neutral axis. It was pure tension by pulling upon the arm in four cases, and in three of the four cases, at least, it was a tremendous stress, and probably so in the other. In all cases the arm was at or above a horizontal. In the case of Frazier, the arm was raised and the element of pure traction was evoked through the lower roots. In no other way can the escape of the 5C root be understood. In our opinion, there would always be in any real case of avulsion, mild or severe, cord symptoms which would be diagnostic. A modified syndrome of Brown-Sequard should be present below the spinal level of the lesion.
Detail of Nerve Paths in the Plexus.
Now that we have seen how traction may be distributed and, through the integrated cord, affect one root or another according to the direction of the pull, it is time to consider the detail of the nerve paths through each root and cord to individual muscles.
Such knowledge as we have of the distribution to the various muscles of the arm of the nerves which form the plexus, has been obtained with much labor in the past by those who approached the problem in three different ways, namely:
(1) Dissections on the cadaver to determine the exact anatomic pathways of nerve fibers from the spinal cord through the intricacies of the plexus to each muscle.
(2) Study of the cases recorded in the literature where definite paralyses of the different muscles have been recorded, and later were shown, by operation or autopsy, to be due to definite lesions of the plexus.
(3) Experimental studies in animals where lesions were made by operation and the resulting paralysis in the muscles carefully recorded, or where electric stimulation at different points in the plexus caused contraction of individual muscles.
Much of our knowledge has come from studies made by Paget, Jonathan Hutchinson, Dej erine-Klumpke, Herringham, Seeligmul-ler, Erb, Duchenne, Bardenheuer, et al., in the era prior to the general adoption of antiseptic technique in surgery, a discovery which so broadened the interests of medicine that other fields more promising than plexus injuries were opened up. However, there is always some one interested in every problem, and to this one Harris, Sherren, Sherrington, Claude, Marie, Thomas, Henri Meige, et al., have made notable contributions in more recent years. It has interested me to make a thorough review of the literature, to collect and study as a group all of the reported cases I could find, and to compare the various diagrams of the plexus presented by different authors, especially those of Kocher, Harris, Kerr, and the many anatomists. While the diagrams present a notable unanimity in general, there is much disagreement in detail, owing to the fact that there actually exists a considerable degree of anatomic variation.
To satisfy my own mind I have made ninety-two dissections of the plexus and have recorded my findings. Fig. 65 shows what I believe to be as accurate a diagram as can be made of a structure which is subject to so many minor variations and which, as those of us who have made dissections best know, may be so easily altered or distorted by our own manipulations.
FIGURE 65
This chart was made personally by Dr. Stevens, as well as the notes which accompany it.
I have not attempted to correct, or in any way change, the chart, although the terminology is not the one in use by anatomists at the present date. Dr. Stevens was accustomed to the old terminology, but in some instances used the more up-to-date one. I believe that any earnest student of this subject could change these terms as accurately as I might. If I attempted corrections I might make a mistake, for I am not as learned in the subject as was Dr. Stevens, although there are some obvious errors in minor details. As the notes were unfinished I have been obliged to correct them to some extent, although I have not checked them with the writings of the authorities quoted.—E. A. C.
In this scheme only dominant roots, or branches which have a large part in the innervation of the individual muscles, are given consideration.
NOTE NO. 1.—The Coraco-brachialis, according to Piersol, is supplied from the 7C root; the Manual of Neuro Surgery, issued by the War Department, 1919, states from the 5C root. Harris in his "postfixed plexus" gives an 8C branch, but there is no record in the literature of a lower root injury accompanied by paralysis of the coraco-brachialis. I have never seen such a connection in the cadaver. Braus gives 6C and 7C. Spalteholz gives 6C and 7C, with 7C dominant. I believe 6C and 6C in many cases (and when so, the 5C and 6C are dominant), but more often it is from the 7C, in which case the 7C.becomes the dominant root. Many times it comes from the 5C, but probably usually is from the 7C via the pathway to the lateral fasciculus. At times there is a branch from the intermediate fasciculus to the coraco-brachialis by another pathway, as given by Harris.
NOTE NO. 2.—The Manual of the War Department gives the Adductor Pollicis as from the 6C and 7C root, which is, of course, quite impossible, except via a lateral ulnar head. Other anatomists give the 8C and ID, which is probably right, and to this we adhere. Stewart gives 8C and ID; Herringham, 8C; Harris, ID; Braus and Spalteholz, 8C and ID. The dominant root is the ID. See Recaldoni and Pfeiffer and Ransom cases.
NOTE NO. 3.—Pronator Quadratus. War Department gives a 6C in addition to the 8C and ID, and Piersol gives the 7C in place of the 6C of the War Department. Herringham gives 7C, 8C and ID. Braus, 7C-8C and ID. I am convinced that it does not come from the 7C. 8C is dominant and the influence of ID is little, if any; therefore it is not given on the chart.
NOTE NO. 4.—The 1st and 2nd Lumbricales are given by Piersol as 6C and 7C. War Department only the 7C; Herringham, 8C; Stewart, 8C and ID; Harris, ID; Spalteholz, 7C-8C-1D; Braus, 8C and ID. Our scheme is the 8C and the ID, for all the lumbricales, and ID is dominant for the 3rd and 4th lumbricales.
NOTE NO. 5.—The War Department gives the Plexor Carpi Ulnaris as having a 7C branch. If so, it would have to go via the decussation to the lateral fasciculus, and could not possibly reach the ulnar, save by the lateral ulnar head. We have, therefore, in our scheme given the 8C and ID (perhaps). Influence of ID must be little, if any, so it is not included on the chart. The lateral ulnar head in our opinion is only sensory from the 7C. Braus gives 7C-8C and ID; Stewart, 7C; Harris, 8C and ID; Herringham, 7C-8C-1D; Spalteholz, 8C and ID.
NOTE NO. 6.—The Flexor Longus Pollicis is given by the War Department as GC and 7C; as 8C and ID by Piersol; Herringham, 7C-8C and ID; Harris, 8C and ID; Stewart, 7C; Spalteholz and Braus, both 6C-7C-8C. We have adhered here to the 8C. No cases of injury to the lateral fasciculus or upper roots have ever been reported as showing injury to the flexor longus pollicis; and where the ID has been involved, the flexor longus pollicis has usually not been included.
Notes continued on back of chart.
NOTE NO. 7.—The Interossel are given by the War Department as having A 7C branch, which we believe impossible, save in rare cases where the 7C gives a branch to the medial fasciculus. Stewart gives 8C and ID; Herringham, 8C; Harris, ID; Spalteholz, 7C-8C-1D; Braus, 8C and ID. I believe 8C and ID is more likely to be correct, ID being the dominant root.
NOTE NO. 8.—The War Department gives the (Flexor Brevis Minimi Digiti, O. T.) Flexor Brevis Digiti Quinti, B. N. A., and the Opponens Digiti Quinti (Op-ponens Minimi Digiti, O. T.) as having a 7C branch, which it seems to me is unlikely. Spalteholz and Braus both give 7C-8C-1D. We favor 8C and ID, and ID is dominant
NOTE NO. 9.—Flexor Brevis Pollicis. The inner head is innervated by the ulnar. In our scheme this head is considered as one of the interossei; therefore inner--vated as the interossei. The outer head is possibly 8C, and, if so, the nerve-path must go via the inner head of the median. Spalteholz, 7C-8C-1D; Braus, 6C and 7C; I favor 8C and ID.
NOTE NO. 10.—Palmaris Longus. The War Department gives 7C, 8C and ID; Piersol gives 6C. Probably 8C takes a straight course to the median, and this is the scheme to which we have adhered. The flexor carpi radialis is given in the Tinel Syndrome as of the outer median head. The flexor carpi radialis and the palmaris longus are innervated probably from the same roots, although it is certainly not the 5C and 6C. They may at times be supplied from the 7C, via the outer median head, but Marie and Meige in electrical stimulation of the outer median head in sixty-four cases caused contraction only of the pronator radii teres (O. T.); of the inner head, they caused contraction of the flexor carpi radialis, the palmaris longus and the other flexors of the wrist and fingers. From our analysis of cases we believe the dominant root for these two muscles to be the 8C, and we so give it. If at times it is the 7C, then in those few cases the path might go via the outer median head, but we believe that this must be rare. The flexors and extensors of the wrist are given by Stewart as 6C, and of the fingers as 7C, which we believe incorrect. Harris gives flexor carpi radialis and palmaris longus as the 8C, as we do. Herringham, 7C-8C-1D, which is unlikely. Spalteholz, the 7C-8C-1D for palmaris longus, and the 6C-7C-8C for the flexor carpi radialis. Braus, the 7C and 8C and ID for the palmaris longus, and the 6C-7C-8C for flexor carpi radialis. Our scheme gives the dominant root for the palmaris longus, the flexor carpi radialis, the flexor sublimis and the flexor profundus as the 8C. If there is a 7C branch, at times, it is not dominant usually, and neither is the ID, which, nevertheless, probably gives a small connection. Therefore, only the 8C is given in our chart.
NOTE NO. 11.—Latissimus Dorsi. The War Department gives 6C and 8C. Piersol is probably more correct, 7C and 8C roots. The only difference would be the presence of latissimus dorsi fibers in the cephalic division. Otherwise the course is the same, but the main nerve is the 7C. In many of our ninety-two dissections the 5C and 6C could have sent no branch to the thoraco-dorsal nerve. Purves Stewart gives 7C, which we know is not so, except in part; Harris as 8C-1D in postfixed, but he gives a 6C in prefixed; Herringham, 6C and 7C; Spalteholz and Braus both 6C-7C-8C. Our scheme gives 7C and 8C.
NOTE NO. 12.—The Teres Major may be innervated by way of the axillary, and this is sometimes the case. The upper subscapular, from the 5C and 6C and posterior division of the 7C, usually goes to the upper part of the subscapularis. The middle subscapular goes to the subscapularis also. The thoraco-dorsalis goes to the latissimus dorsi, and the axillary subscapular supplies the teres major'. Spalteholz gives 5C-6C-7C for subscapularis, and 6C and 7C for the teres major. Our scheme is the same for the subscapularis, but the 7C and 8C for the teres major.
NOTE NO. 13.—The radial extensors of the wrist, it must not be forgotten, are supplied sometimes by the 5C (see Harris and Low, Fairbanks and Sherren), but more often probably from SC-6C and 7C. In an analysis of the twenty-four cases of cut 5C, or 5C and 6C roots (not tension), the extensor carpi radialis longus and brevis were involved, or reported involved, only seven times, so they are not always from the 5C and 6C, therefore probably 7C; Herringham, 6C and 7C) Harris, 5C and 6C; Stewart, 6C; Spalteholz, 6C-7C-8C; and Braus, 6C and 7C. Our scheme is the 5C and 6C at times, and these are dominant. When from the 7C, as they often are, the latter is the dominant root.
NOTE NO. 14.—While many muscles possibly have a small branch supply from the 6C, it is generally admitted that there is little extension of the paralysis produced by involvement of the 6C when the 5C is already involved. Direct stimulation of 6C causes contraction of the clavicular portion of pectoralis major, posterior part of the deltoid and some of the forearm muscles, probably pronator radii teres. Stewart gives the pectoralis major as 6C-7C; Harris as 5C-6C; which it certainly is at times. Spalteholz gives it as the 5C-6C-7C-8C; and the pectoralis minor as the 7C and the 8C. Our scheme gives the pectoralis major as the 6C-7C and 8C, and the pectoralis minor as the 7C and the 8C.
NOTE No. 15.—All the flexors and abductors of the thumb, and all the extensors of the thumb, are given by various authors as having a 6C branch. Both Piersol and the War Department give the abductor pollicis as 6C-7C, as does Braus. Spalteholz gives the thenar muscles as the 6C-7C and 8C, and even ID for the opponens pollicis. Tinel specifically says paralysis of the abductor pollicis, the opponens pollicis and the flexor brevis pollicis is evidence of injury of the inner median head and therefore from the caudal roots. Very rarely have any injuries to the lateral fasciculus or cephalic roots been accompanied by disturbance of thumb action, and for that reason we have not given a 6C origin to any of these nerves. The flexors and abductors of the thumb are innervated by the 8C and ID, through the inner head of the median, and the extensors of the thumb by the 7C and 8C, dominantly at any rate. Andr6 Thomas and Leverty are the only authors mentioning an involvement of the thenar muscles in an upper root lesion. Braus gives the opponens pollicis and flexor brevis pollicis as 6C and 7C, and the adductor pollicis as 8C and ID. Our scheme is 8C and ID for flexors, abductors and adductors of thumb; for extensors of the thumb 7C and 8C, with a small connection from ID at times, which is not dominant, and therefore not included in our chart. The abductor pollicis longus (B. N. A.), it must be remembered, is the extensor ossis metacarpi pollicis of the old terminology as it is called in this chart. Its innervation is via the radial from the 7C and 8C, and it is considered here as an extensor. Nevertheless, in a pure median paralysis through its action, the thumb may still be abducted.
NOTE No. 16.—The Pronator Radii Teres is often supplied from the 5C or the 5C and 6C. Many times probably from the 7C, when not from the 5C or 6C. Sherren says that in his Erb-Duchenne type he never saw the pronator radii teres involved. In two of Harris' cases it was involved, and in two of Andr6 Thomas'. These were skilled observers. In our series it was involved with a 5C, a 5C and 6C, and a 6C cut, so it certainly comes from the upper roots, at times, but that it does not always do so, is evidenced by our list. In Apert's case with a 7C-8C-1D involved, all the epitrochlear muscles were a mass of fibrous tissue, While the epicondyiar were in good condition. So probably the pronator radii teres is at times from the 7C. Braus gives 6C and 7C.
Animal experimentation has been of some value, especially on monkeys, but the differences from the human have prevented very much advance from this direction. I do not feel that I have myself derived enough benefit from articles on this phase of the subject to review them here. The anatomic method giving the best results has probably been the examination of the macerated fetal structure and the tracing of individual nerve fibers through the intricacies of the plexus. This was the method used by Herringham. The anatomic charts which we have incorporated here have many points of difference from those which have been published by various authors and anatomists. The root scheme which we have found helpful, differs quite markedly from most of those published, including those of Tinel and Benisty, Henri Meige and Purves-Stewart among the neurologists, and of Piersol, Gray, Spalteholz and other anatomists. Some of the reasons for these differences will be found in the notes attached to the charts, or in the text. Figure 65 will give the reader our idea of the root innervation and of the ordinary arrangements of the plexus better than a detailed description, bearing in mind always that this representation is only schematic, and does not resemble in the least what the surgeon sees in dissection as he comes down upon it from the supra- or infra-clavicular incision.
Prefixed and Postfixed Plexuses.
There have been several classifications of the varieties of the brachial plexus. Harris's division into prefixed and postfixed types has been very generally accepted and used by anatomists and neurologists. Briefly, the prefixed type has a 4C connection to the 5C and no 2D to the ID, while the postfixed plexus has a 2D connection to the ID and no 4C connection to the 5C, therefore making them essentially different types, which do not overlap. This would be of little practical importance, if true, since even its authors do not claim that it raises or lowers the individual root constituents of the plexus one whole vertebral segment. There are other minor individual nerve difference;.! in this classification, but these are the essentials. I doubt the importance of this classification and give my reasons as follows.
In our 1930 series of sixteen plexuses there were four with small connections from the 4C to the 5C root, as usually described. In three of these prefixed plexuses there was also a 2D connection making them, at the same time, postfixed plexuses; but both of these connections were small. This was not all. By careful dissection I found in eight plexuses another small connection, apparently from the 4C, which ran down through the foramen transversarium, beside the vertebral artery, to join the 5C root outside the transverse process. I was unable to find any record of such a nerve in the literature. I traced it into the spinal canal at the 4C. In no case did it come from the sympathetic trunk, so far as I could determine, and I cannot believe it to be a fiber which comes out with the 5C root beyond the transverse process and then turns back to become part of the sympathetic nerve, which constitutes the so-called vertebral nerve of the sympathetic, described years ago by Vulpius and Francke. I regard it as another small connection from the 4C to the 5C. In six of the eight, it was present with a 2D to the ID. In the two others, the 2D to the ID connection, it was probable, although it could not be determined absolutely, as against a connection with the sympathetic alone, since the relation was too close to permit of a decision. The 2D connection to the ID was sometimes separate, but usually connected with the sympathetic branches to the first thoracic ganglion. In several it was impossible to tell whether or not it was a 2D connection to the ID, or a branch to the ganglion. The thorax always has to be opened in order to be sure of a connection from the 2D to the ID. In the sixteen dissections a 2D connection was present in ten cases, and impossible to determine in four others.
I believe, if carefully looked for, there is in the maj ority of cases a small 4C connection to the 5C, and also a small 2D connection to the ID. This is of importance, especially since the operation of stellectomy has come so prominently to the front. Injury during removal of the stellate ganglion to this 2D connection to the ID, when it exists, may be accompanied by some minor paralytic involvement in the ulnar distribution in the intrinsic muscles of the hand.
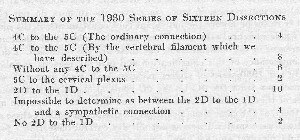
I submit that with these findings, the idea of a prefixed and postfixed plexus must be rejected, because if a plexus is prefixed it certainly cannot be postfixed, even as a distinctive academic type. If we accept the presence of this vertebral nerve filament which we have described, we have ten plexuses out of sixteen dissections with a 4C connection of some kind to the 5C, and also ten with a 2D to the ID and eight with both. With this proportion, any classification based on the presence or absence of a 4C connection, or the presence or absence of a 2D connection to the ID, would seem to us artificial, unnecessary and misleading.
The posterior connections to form the intermediate fasciculus usually come from the roots individually, but the amount of fascia left unremoved may account for different opinions. In the sixteen cases of the 1930 series freed from enough fascia, we found that they not only come from the roots behind their junction in the case of the 5C and 6C, but the same arrangement holds good for the 8C and the ID. However, in sixteen plexuses the ID failed to send a connection to the intermediate fasciculus six times. It was nearly always small, even when present. Cunningham originally denied any such connection, as did Testut and Quenu. Herringham states that it is seldom present, yet Harris found such a connection in eighty-two per cent of his cases, and Kerr found it in 169 of his 175 plexuses.
Classification of Anatomic Variations in the Brachial Plexus.
Obviously no such single diagram as Figure 65 can be utilized for every instance of brachial plexus injury, for almost every individual plexus would differ in some detail from any standard we might set. However, we may attempt to classify the most common and important variations in the hope that in time we may be able to understand exceptional cases of paralysis. These variations have been classified especially elaborately by Kerr, and for the sake of brevity, I present his study of the plexus here in a tabulated form, which I have myself arranged from his written descriptions.
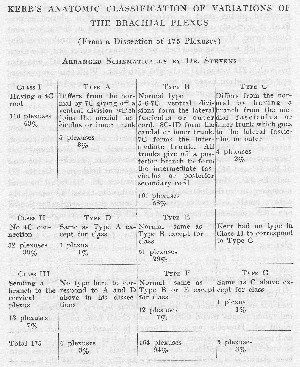
This chart gives as comprehensive an idea of these different types as I can find, but we must assume, as he does, that the types do not overlap, although this is evidently not strictly true. His divisions are perhaps useful for anatomic study, but must be greatly simplified to be of use to the practical surgeon.
The normal type (Types B, E, and F of the chart belonging to Classes I-III) includes 93.7 per cent of all his dissections, and Classes I and II include 91.58 per cent, or all but thirteen cases in which there was a branch to the cervical plexus. This last is an artificial distinction, and to me it seems more simple to classify the plexuses as I have below. Certainly the normal type should be Type A to facilitate remembering the different types.
Whether or not there is a small ascending connection, consisting of one or two filaments at most, to the cervical plexus above, on which Kerr bases his Class III, is a matter of no particular importance, even anatomically. In our ninety-two plexuses it was present in only thirteen per cent. In our 1930 series of sixteen plexuses, very carefully done, it was present in two cases, one a fair-sized nerve. Kerr found it in only seven per cent of his series.
In ninety-two dissections, twenty-two of them superficial observations, but nevertheless including the roots, we have never seen a 4C connection to the 5C which was of the size described by Harris, and most of the connections were small indeed. I have never seen a brachial plexus with a 4C connection as large as that represented by Kuntz in his wonderful work on the Autonomic Nervous System, but that is simply a representation. I have seldom seen this connection of a size which would permit of a suture, as has been reported in the literature. In such cases we should gravely question the reports. Especially with scar and infiltrate present, we do not believe that any surgeon could suture this connection in most of the cases as we have found them.
Kerr altogether ignores the presence or absence of a 2D connection to the ID and therefore makes no claims of special types depending on this connection. All his classes are subdivided into types which he designates by letters which do not correspond for the various classes and consequently tend to confuse. His types A and D, depending on a 7C connection to the medial fasciculus, ignore those plexuses which contain a lateral ulnar head, which we contend is probably normal or at least common, and which probably comes from the 7C root, although via the lateral fasciculus where this exists, and certainly goes to the inner median head and to the ulnar, which are the terminal branches of the medial fasciculus. If it goes to the terminal branches of the medial fasciculus, it would seem to be much the same thing as if it went to the medial fasciculus itself. In sixteen dissections we found it present eight times.
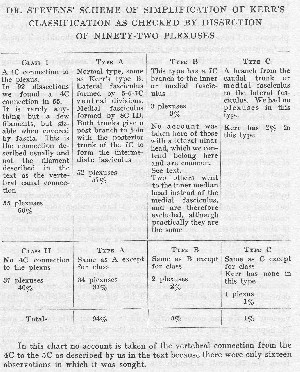
The individual variations of terminal branches which might be the cause of unusual paralyses are many. Of variations in the larger anastomoses in the upper portion, that of the musculocutaneous to the median is the most common. In seventy-five plexuses Kerr reports a connection from the musculocutaneous to the median eighteen times. In two of our last sixteen dissections there was a fused musculocutaneous and median as far as the elbow, and in six others a less extensive connection. In none of the entire ninety-two did we find a connection from the median to the musculocutaneous. Ignoring the smaller connections, in ninety-two plexuses we had eight large connections from the musculocutaneous to the median, where this connection was of such a size as to appear to be the main terminal branch of the musculocutaneous. In three, the junction of the musculocutaneous and the median was just above the elbow. In one, the median outer and inner heads were separate to the elbow, and at this point were joined by a branch of the musculocutaneous, all three being of equal size; therefore, three separate pathways for the median innervation. It may be seen that a peripheral nerve injury involving only one or two of these branches would be difficult to locate. In one dissection the entire musculocutaneous joined the median four and one-half inches below the clavicle. In only one case did we have a connection from the radial to the ulnar high up in the axilla, and in only one was there a connection from the median to the ulnar at the elbow. In the hand and forearm, the median and ulnar often sent small branches of anastomoses. A knowledge of these anomalies may be of use in any case of unusual muscle or sensory paralysis.
The types of brachial plexus, so far as stress is concerned, are three.
Type 1—where the suprascapular comes frankly from the 5C root or by two roots from the 5C and 6C before they join to form the lateral fasciculus. Obviously, a stress here could fall on the lateral fasciculus with a greater chance for the escape of supraspinatus and infraspinatus. There were fourteen such cases in our series of ninety-two, and by removing a little more fascia, it is found that the suprascapular goes back to the 5C root in nearly all cases, sometimes alone and sometimes with a filament or two from the 6C. In one dissection we found a suprascapular entirely separate from the lateral fasciculus, with three branches of origin—4C, 5C and 6C— these branches coming from far back on the roots. The origins from the 5C and 6C were at the exits from the gutters of bone at the transverse processes. In two cases of the entire series, but with a good deal of fascia removed, the suprascapular came directly from the 5C, and the 5C sent no ventral branch to the lateral fasciculus, but only a posterior which joined the posterior of the 6C and 7C. In this case the lateral fasciculus was clearly 6C and 7C, and the musculocutaneous nerve could contain no fibers from the 5C.
In the second type stress might well be transmitted so as to fall strongly or entirely on the 7C root. It is characterized by the fact that the 7C ventral branch passes directly to the outer median head. In fact, the ventral connection of the 7C is the outer median head, although it may receive a filament from the 5C or 6C.
In the third type the 7C ventral division went to the medial fasciculus without any branch to the lateral fasciculus. In such cases any ventral 7C root fibers would have to go via the inner median head or the ulnar, and therefore it is clear that a wound of the medial fasciculus would cause more damage to the median innervation than would be usual, and might even involve the coraco-brachialis when this muscle is innervated by the 7C. There were only five cases of this type in our entire series of ninety-two. In no case of this type did we have a lateral ulnar head. So we assume, as stated above, that the lateral ulnar head is probably from the 7C.
The last two of these three types were so small in number as to be negligible, except in an intensive anatomic study of the plexus. Therefore, in the majority of injuries, stress might not fall heavily on the suprascapular nerve.*
*In such cases the arm might be abducted by the action of the supraspinatus alone.—E. A. C.
Recorded Cases of Rupture or Division of Parts of Plexus.
The diagram of the plexus which I present as possibly an improvement on those of other authors has also been checked or modified from a study of 710 cases of brachial plexus injury from the literature. In arranging the root charts of muscle innervation, we have utilized the information obtained by an examination of the reports of paralyzed cases in which the exact pathology was known. There were some cases where, with cut or ruptured upper roots, it was possible to draw fairly accurate conclusions as to the innervation of muscles from those roots. A careful examination of the table, representing muscle paralysis, with cut or ruptured 5C, or 5C and 6C, or 6C roots alone, will, we believe, bear out our statement. Although these observations were mostly recorded by trained men, many were not neurologists trained in electrical reactions, and it is likely that reports as to the condition of certain muscles are not included. Such a conclusion cannot apply to men like Andre Thomas, Harris, Sherren, Thorburn, Head, et al., whose cases are included.
The degree of involvement of the muscles supplied by the collaterals arising near the roots, should be considered in the differential diagnosis of a root lesion. We believe that this is most important, and that a report should state their condition. Many times this information will clear up a seemingly complex problem. Nevertheless, even the reports in this selected series of twenty-four cases, many of them from masters of neurosurgery, show how few times the muscles supplied by these collaterals were definitely recorded as injured or as not injured. It seems highly probable that their condition was ignored in some cases, and that if their condition had been carefully examined, paralyses would have been found more often.
In the case of the lower roots the same method was pursued, but here it was more difficult, as there was no case of frankly cut or even injured 7C alone, except Mingazzini's case. The Dejerine-Klumpke type has been seldom checked by operation, except in the four cases where it formed part of a complete paralysis, and no root conclusion could be drawn.
The cases of Recaldoni, Pfeiffer, Ransom, Gosset and Quenu, et al., which, while not of cut roots, were at least involvements of the 8C and ID in pathological processes, were also utilized, together with many others, in arriving at what we believe to be at least an approximation of the muscle innervation of the lower roots. The rest was by exclusion, e.g., many cases were reported as injuries of the 5C, 6C and 7C. Not one of these included the paralysis of either the flexor carpi radialis or the flexor longus pollicis. Therefore, we assume that these muscles do not receive their nerve supply from the upper roots.
The table of twenty-four cases where the lesion was known and the paralyses were of Erb-Duchenne type is interesting as a diagnostic study. It tends to prove that no distinction can be drawn between lesions of a 5C, a 5C and 6C, or a 6C lesion alone. It shows how little weight is to be placed on the lack of the report of involvement of the root collaterals even in a frankly Erb-Duchenne type. On the other hand, paralyses of the supraspinatus, infraspinatus, deltoid, biceps, brachialis, and brachioradialis may be confidently expected, as shown here, always to occur in this form of paralysis. If the muscles supplied by the root collaterals are paralyzed, it helps the diagnosis, but this table clearly shows that if they are not included, it just as certainly does not rule out a complete lesion of these upper roots.
There were twenty-four cases involving the 5C or 6C, where we could localize the injury sufficiently for our purpose. In two of these the 7C was also slightly involved, but not enough to be of much importance, so they are included. One of these had a slight involvement of the triceps, but the other was purely Erb-Duchenne. One other case not included in the twenty-four, Winnen's case, involved a 4C connection to the 5C, at the point of junction, it was said.
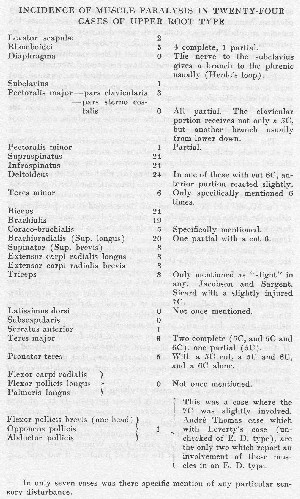
Conclusions from Analysis of 710 Reported Cases.
In the series of cases from the literature, beginning with Flaubert in 1827, I found that many were of little importance, since the details were too meager to give us much information as to the methods of production, or even the exact muscle paralyses, and in most of them there was no operation or autopsy by which to check. With all the World War wounds, it would seem that there should have been details in an immense number of cases. Such, unfortunately, was not true. Thousands of cases of peripheral nerve wounds, and some in great detail, were reported, but where the brachial plexus was concerned, the description of the operation in most cases was confined to the wounds, with no detailed account of- work on the plexus itself.
These cases were reported by many men. Gosset—fourteen. Moynihan—eleven cases of brachial plexus; four upper, seven lower. Tuffier—280 operations on nerves, but no brachial plexus. Boinet— twenty-five cases of brachial plexus injuries. Tinel—in 639 nerve lesion reports, twenty-seven brachial plexus. Price, Feiss and Terhune —sixty cases of brachial plexus injuries; five complete. Mauclaire— four cases, one axillary, none of them complete. Chiray and Roger, Leclerc, Benisty, Fere, Wiart, et al., reported others. In all, there is a lack of detail, so that we can get very little help from their analyses for our particular purpose.
In 710 case reports examined, there were 135 cases in which an operation or autopsy had been done.
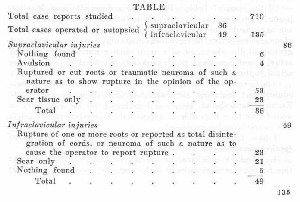
Let us analyze the eighty-six supraclavicular injuries in order to avoid the fallacious conclusions which we think other students of the subject have come to. Eighty-six cases of supraclavicular rupture would seem a large proportion of the 135 cases on which operation or autopsy had been done. Doubtless among the remaining 575 which were unchecked, and in which no conclusions could be drawn other than the incidence of paralysis, the proportion of supra- to infra-clavicular injuries might have been the same, but as to that we can only theorize. To determine the cases of actual rupture, we must exclude the following fifty-four cases from the eighty-six supraclavicular injuries.
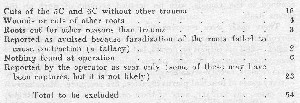
This leaves only thirty-two cases which represent instances of trauma other than cuts or wounds, where roots were reported as separated either because the two ends were found, or because the traumatic neuroma or scar was of such a nature as to lead the operator to believe that such was the case.
Of the cases of Tubby, Tuffier, Bardenheuer, Bristow, Hartley, Banks, Thorburn, Sherren, Kalb, Fisk, Ginsburg, and Thomas, there can be no doubt; we may include also the four cases of avulsion; but of some cases where the report was made of a neuroma or a disintegration of the plexus, or of scar of such a nature as to prevent actual knowledge, there is grave doubt, not of injury, but of an actual rupture of any part of the plexus.
The German and Austrian literature has been examined less thoroughly, but including Bernhardt, Wolfler, Winnen, Erb, Kalb, Kramer, Bardenheuer, et al., and excluding all the cut roots or wounds, we have been able to accept only thirty-two cases as definite supraclavicular ruptures!
I have found only four proven cases of rupture de la moelle epiniere (avulsion) in all the history of medicine.
- Flaubert of Rouen, France, 1827. Reduction of a dislocation by the combined force of eight men. All roots except the 5C ruptured from the spinal marrow and recovered below the clavicle at autopsy. Death on the fourth day.
- Apert, France. Boy, arm caught in the wheel of a heavy cart; thrown over and over. Autopsy thirty-two and one-half years later. Complete rupture at the spinal cord of the 7C and 8C and the ID. No ascending degeneration of spinal tracts, but the brain area was smaller.
- Boyer, Toronto, Canada. Birth case. Arm pulled. Rupture more pronounced of the 7C, but 5C-6C-8C and ID are included as injured. Ascending degeneration marked. Brain area involved smaller. The autopsy was made forty-one years after the injury.
- Charles Frazier, Philadelphia. Man struck by another man falling three stories; 6C, 7C and 8C ruptured, from the spinal marrow. Laminectomy, for intolerable pain, afforded the opportunity to study the exact seat of the injury. Dr. Frazier cut the ID and the 5C sensory roots. In this case there was a suspicion of a fractured vertebra.
These are the only four cases I can find in the literature with proven avulsion, but these cases have been responsible for the misconception that the usual locations of injuries to the plexus are within the spinal canal or in the bony gutters proximal to the snubbings on the transverse processes.
Treatment.
Of the non-operative treatment little need be said except that a paralyzed muscle recovers quicker when not in a condition of stretch. One must know and analyze the individual muscle paralyses in order to meet this indication. If one learns to prevent contractures which follow in these paralyzed cases from over-action of muscles not paralyzed, he will have gone a long way in the intelligent treatment of brachial plexus injuries. In cases of complete interruption of the nerve paths, contractures are usually soft and reducible. Only in irritations do we get the hard, irreducible griffs, and these must be prevented by treatment. It is easier than to correct them after they have occurred—in the domain of the median, the accoucheur's hand; in the domain of the ulnar, the claw hand; in the domain of the radial, the wrist drop.
Operation.
Immediate operation is indicated in all cases of penetrating wounds with paralysis involving the branches of the plexus, and in all cases showing the complication of subclavian or axillary arterial injuries. The presumption should be against operating in cases of tension or traction injuries. Were I to select the factor of most importance in determining the question of operation, I should wish to know the manner of the trauma. Lesions of the plexus accompanying dislocation and near dislocation will rarely cause actual rupture, and, therefore, may recover as well without operation as with it. The chance of suture of a ruptured nerve trunk is a forlorn hope. The main indication for operation is the release of pressure from exudate. The resection of a nerve simply because it has a traumatic neuroma or local enlargement is unwarranted;- there must be clear evidence of entire anatomic separation. False neuroma is often hard to distinguish from true, and it will many times interrupt the electric current. See Henri Claude, Dejerine, et al. Lysis, simple longitudinal incision, as taught by Bardenheuer long ago, will give the greater percentage of cures, and resection should be reserved for those cases showing actual separation. The time to operate in secondary cases is of importance. Some say three months, but there are many cases that will not begin to show first motor return in that time, and therefore, if operation were to be the rule, it would be better to operate at once. In expert hands immediate operation is justifiable in any doubtful case, but a surgeon without a knowledge of the local anatomy and general history of the subject might easily do harm. In most cases recovery of function begins within seven or eight months, but many cases have recovered first motion at a later period. In one of my cases, a root lesion due probably to abduction and external rotation during a breast amputation, the first voluntary motion appeared at the end of five and one-half months. Faradic contractility and voluntary motion were noticed on the same day. The best argument for not operating in tension injuries is that actual rupture of the brachial plexus is a rare condition, although temporary palsy is common. The reason is that the stresses do not fall entirely on the brachial plexus as in our theoretical traction apparatus. After the bones and ligaments are separated, stresses are distributed to all the fascial investments of the axilla and neck and so disseminated. Much of the strain, especially when transmitted from below, is taken up by the tendons as evidenced by rupture of the long head of the biceps, so often observed in dislocations and in fractures of the upper end of the humerus. Always, as explained on p. 348, there are small tears and injuries of the fascia about the nerves and vessels, and probably also far removed along the fascial planes. There are petechial hemorrhages and exudate which surround not only the roots but the cords of the plexus in both the supraclavicular and axillary regions. But if rupture occurs, it is at the roots or of terminal branches and not of the plexiform part, which, nevertheless, may be swollen by pressure of the exudate within the fascia surrounding it.
Some Practical Rules in Diagnosis for Use with Chart.
There are many exceptions, but the following points will usually hold good.
If in an upper type lesion the brachioradialis is involved, it is usually a lesion of the 5C or 6C roots.
If the brachioradialis is not involved in a purely radial or extensor paralysis, often entire at first but later only partial, it is a lesion of the 7C. In such a case the coraco-brachialis, when it comes from the 7C as it often does, would be the only flexor in the upper arm paralyzed and would become the key muscle.
It must not be forgotten that in the wrist drop from paralyzed forearm extensors due to lead poisoning, the integrity of the brachioradialis and supinator is almost diagnostic, and this condition must be excluded.
If all the extensor muscles of the arm and wrist and fingers, and the brachioradialis and supinator also are paralyzed, it is a peripheral lesion of the radial nerve.
If only the deltoid and teres minor of the upper group in addition to the above are involved, it is a trunk and not a root lesion of the intermediate cord or a peripheral lesion of two nerves—radial and axillary.
If it is a combined paralysis of the flexors of wrist, thumb and fingers, except the brachioradialis and the pronator teres, and all extensors are involved, it is a lesion of the 7C and 8C and ID.
If the lesion is as above but only partial of the triceps, the latis-simus dorsi and partial of all the extensors of the wrist and fingers, with escape of the brachioradialis and extensor carpi radialis longus and brevis, it is a lesion of the 8C and ID roots.
If the paralysis is of all the flexors of wrist, thumb and fingers with the exception of the brachioradialis and the pronator teres with escape of the triceps, anconeus and all extensors, it is a lesion of the medial fasciculus.
If only the ulnar flexors of the forearm are involved and all the hand muscles except the opponens pollicis and the abductor pollicis brevis and one-half the flexor pollicis brevis, it is a lesion of the ulnar.
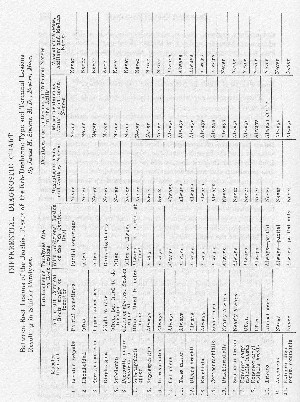
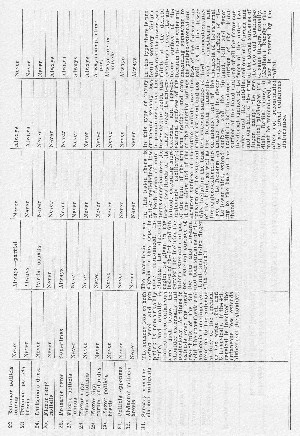
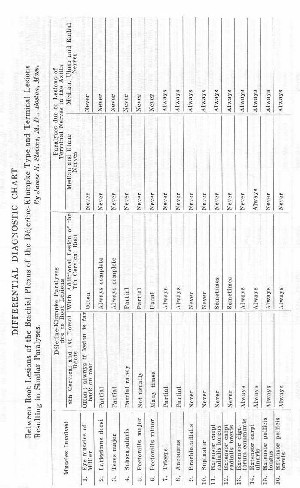
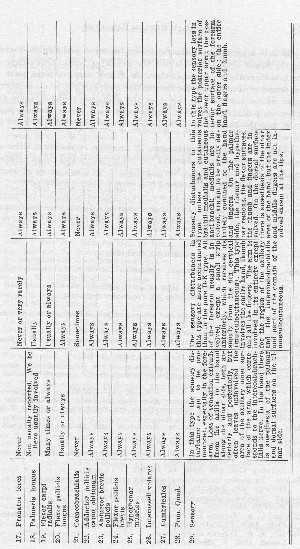
If it is a paralysis of the flexors of the wrist and fingers, including the flexor longus pollicis and the pronator teres, with escape of the brachioradialis and supinator, the flexor carpi ulnaris, part of the flexor profundus digitorum and all interossei, it is a peripheral lesion of the median. In this case the abductor pollicis brevis and opponens pollicis and part of the flexor pollicis brevis are also paralyzed, but the hand muscles and adductors of the thumb are not involved.
The abductor pollicis longus, it must be remembered (the extensor ossis metacarpi pollicis of the old terminology), is an extensor innervated by the radial. Nevertheless, it may act as an abductor of the thumb. It is not involved in a pure median paralysis.
Care must be taken not to confuse a root lesion with a peripheral paralysis which involves two or more nerves. In such a case diagnosis is more often difficult and will tax the knowledge of the observer.


