Instability Classification (Stanmore)
THE CLASSIFICATION OF SHOULDER INSTABILITY - NEW LIGHT THROUGH OLD WINDOWS
Courtesy of: I. L. Bayley, Royal National Orthopaedic Hospital
There are broadly two reasons why shoulders become unstable. In the first, there are structural causes, either because the capsulolabral mechanisms have been damaged by a major injury, or because the capsulolabral structures are already deficient, predisposing the shoulder to develop instability as a result of minor injury or repetitive micro-trauma or as a result of some action such as throwing a ball. The second cause is that of the development of unbalanced muscle recruitment around the shoulder - as opposed to muscle weakness - which result in the humeral head being displaced upon the glenoid. However the classification of shoulder dislocation is controversial. Systems tend to be fragmented and idiosyncratic and there are so many in use that it is difficult to compare the result of treatment from one reported series to another. Confusion is compounded by the frequent misunderstanding of common terms. For example multi-directional instability, which is a symptom and not a diagnosis, means one thing to one doctor and quite something else to another, the terms voluntary and involuntary are particularly hard to differentiate; confusion often exists as to whether a shoulder is, in fact, unstable or just plain lax. Neither do existing classifications recognise two fundamental issues, namely that a combination of pathologies may exist and also that cases may move from one group to another over time.
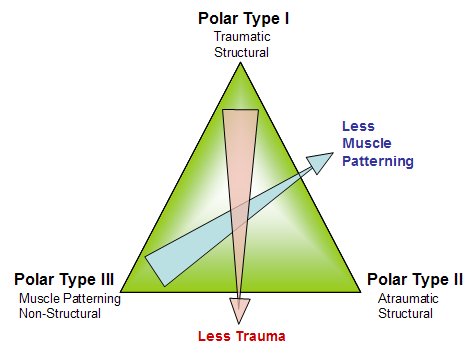
The system of shoulder dislocation classification which we have developed at the Royal National Orthopaedic Hospital and used over the years is anchored by three basic or polar groups:
I Traumatic structural
II Atraumatic structural
III Habitual non-structural (muscle patterning)
The system works well for posterior and anterior dislocations and also for subluxations, and complete dislocations. It can be expanded as follows:
I Traumatic structural
a) acute
b) persistent
c) recurrent
II Atraumatic structural
a) recurrent
III Habitual non-structural
a) recurrent
b) persistent
The diagnosis of each type is made on the basis of a careful history and clinical examination followed by arthroscopy and, when necessary, functional electro-myography. I shall show examples of each type. The history takes account of the degree of trauma required to cause the first dislocation and whether the displacement was complete and requiring formal reduction or incomplete and spontaneously reducing. The clinical examination looks for signs of ligamentous laxity and specifically for evidence of abnormal muscle pattern recruitment. The presence or absence of articular surface damage is defined by arthroscopy and functional electromyographic studies look for evidence of abnormal muscle pattern recruitment in patients in whom clinical examination has been negative but suspicion of a non-structural instability is high. The characteristics of each of the three polar groups are broadly as follows:
I Traumatic structural
• significant trauma
• often a Bankart’s defect
• usually unilateral
• no abnormal muscle patterning
II Atraumatic
• no trauma
• structural damage to the articular surfaces
• capsular dysfunction
• no abnormal muscle patterning
• not uncommonly bilateral
III Habitual non-structural (muscle patterning)
• no trauma
• no structural damage to the articular surfaces
• capsular dysfunction
• abnormal muscle patterning
• often bilateral
Similarities between polar groups II and III will be self-evident. Furthermore, a careful doctor when examining patient’s in clinic and investigating them by arthroscopy will soon discover that there can be much overlap between groups. For example, some patients in polar groups III do give a history of injury of varying degrees of severity. Other patients will have a clear cut muscle patterning problem and will also demonstrate clear cut articular surface damage at arthroscopy. Appreciating these variations it becomes clear therefore that in addition to some patients fitting securely into the three polar groups, there are others that seem to have — and indeed do have — a dual pathology.
One could perhaps characterise this situation by drawing three overlapping circles. However this model tends to compress the interlocking parts of the circles and might compound rather than relieve confusion. We have preferred to use the model of a triangle since it better highlights the continuum of presentation which can occur in between the three polar groups. It is possible to fit patients into the three polar groups or somewhere along the lines which join them.