Platelet Rich Plasma (PRP)
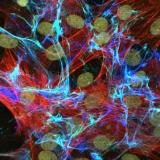
Growth Factors are an essential part of the body's healing process. These are molecules that trigger the various stages of the healing of tendons, ligaments and bones.
When injury occurs, the damaged cells and exposed collagen proteins stimulate an inflammatory process. Platelets are the first cells to arrive at the injured site and release growth factors which start the healing process. This is followed by leukocytes (white blood cells) which also release growth factors. The white cells then start clearing the site of debris. At about 7 days growth factors activate fibroblasts to produce type 3 collagen forming a strong scar tissue. After about 21 days the scar tissue starts to be replaced with normal tissue (type 1 collagen) and the healing process proceeds to completion.
Since platelets found in blood are a very rich source of growth factors scientists have worked at utilising platelets from a patient's own blood, by isolating, concentrating and activating the platelets to increase the growth factor content four fold. In addition, useful white cells are also included to assist healing further by reducing inflammation and fighting infection. This is known as Platelet Rich Plasma (PRP). For details on the growth factors in PRP click here .
Many studies suggest that platelet rich plasma may help in the healing process by concentrating the growth factors all at once in the correct location. PRP has been used since the 1970s, but research and technology have advanced rapidly demonstrating it's advantages and applications for many tendon and bone injuries.
Because the materials used in the treatment are derived from your own body, the chance of adverse drug reactions is eliminated, making the process completely safe. In addition, with the use of closed PRP systems, no other product or material is allowed to enter during the PRP production process. The systems can also be completely automatic, which allows for consistent reproducible concentrates of PRP.
PRP is currently used for tennis elbow, rotator cuff injuries, muscle injuries, fractures and many other tendon, ligament and bone injuries.
Although there is a large amount of basic science research on PRP, clinical studies are only now appearing in the literature. Therefore it is not widely used by all clinicians and it's exact benefits in the clinical setting are yet to be properly defined.
Also See:
- Related Articles (Google Site Search)
- Education Section
- PRP for Rotator Cuff Tears - our results
- New mechanical insights into healing
- Bloodcure.com
Types of growth factors in PRP
The growth factors name reflect their activity or origin. These are:
1. Platelet derived growth factor (PDGF). It is a protein produced by platelets, macrophages and endothelial cells and stored in the platelets healthier granules. It is released when the platelets group together thus starting the coagulation cascade. The connective tissue cells of this area respond by initiating a replication process.
2. Vascular endothelial growth factor (VEGF). This has immune acid similarity of 24% to PDGF beta but joins different receptors and so provokes different biological effects. It is a powerful mitogene for endothelial cells and produces angiogenic actions in VEVO.
3. Transforming growth factor (TGF). This is a super family of proteins that includes morphogenic bone proteins and others. It has three fundamental functions.
- Modulates cell proliferation (it is a suppressor).
- Increases the synthesis of extra-cellular cell matrix.
- Produces an immune-suppressor effect.
4. Insulin like growth factor Types i and ii. These are found in large quantities in the bone. They increase the number of osteoclastic multinucleated cells. The differentiation and Type I collagen biosynthesis.
5. Fibroblast Growth Factor (FGF). Stimulates angiogenesis, endothelial cell proliferation and collagen synthesis.
6. Connective Tissue Growth Factor (CTGF). Promotes angiogenesis, cartilage regeneration and fibrosis and platelet adhesion  top top
top top
Evidence for the benefits of PRP
Platelet Rich Plasma (PRP) is not a new an experimental technique. It has been widely studied since the early 1980's and the first publication on it's benefits for muscle healing was published in 1986 [2]. Since then there have been many in-vitro clinical studies demonstrating it's benefit in enhancing the healing process in numerous areas of the body:
- Achilles tendon
- Sanchez M, Anitua E, Azofra J, Andia I, Padilla S, Muljika I. Comparison of surgically repaired Achilles tendon tears using platelet-rich fibrin matrices. Am J Sports Med . 2007;35:245 - 251.
- Muscles tears:
- Jodczyk K J, Bankowski E, Borys A. Stimulatory effect of platelet-breakdown products on muscle regeneration. Zentralbl Allg Pathol 1986; 131 (4): 357-61.
- Rotator Cuff
- DeOrio JK, Cofield RH. Results of a second attempt at surgical repair of a failed initial rotator cuff repair. J Bone Joint Surg Am 1984;66:563 - 567.
- PIETRO S. RANDELLI, PAOLO ARRIGONI, PAOLO CABITZA, PIERO VOLPI MD, & NICOLA MAFFULLI. Autologous platelet rich plasma for arthroscopic rotator cuff repair. A pilot study. Disability & Rehabilitation. 2008
- Knee Surgery
- Everts PA, Devilee RJ, Oosterbos CJ, Mahoney CB, Schattenkerk ME, Knape JT, van Zundert A. Autologous platelet gel and fibrin sealant enhance the efficacy of total knee arthroplasty: Improved range of motion, decreased length of stay and a reduced incidence of arthrofibrosis. Knee Surg Sports Traumatol Arthrosc 2007;15:888 - 894.
- Medial collateral ligament of the knee:
- Hildebrand K A, Woo S L, Smith D W, Allen C R, Deie M, Taylor B J, et al. The effects of platelet-derived growth factor-BB on healing of the rabbit medial collateral ligament. An in vivo study. Am J Sports Med 1998; 26 (4): 549-54.
- Batten M L, Hansen J C, Dahners L E. Influence of dosage and timing of application of platelet-derived growth factor on early healing of the rat medial collateral ligament. J Orthop Res 1996; 14 (5): 736-41.
- Tennis Elbow
- Mishra A, Pavelko T. Treatment of chronic elbow tendinosis with buffered platelet-rich plasma. Am J Sports Med 2006;34:1774 - 1778.
There is far more research on PRP in the literature than for most new orthopaedic implants, which often have little in-vitro clinical research before being released onto the market and used by surgeons.  top
top


