Stabilization of the Acromioclavicular Joint
Few issues in orthopaedic surgery are more contentious than the continuing debate concerning operative or conservative treatment for a dislocated acromioclavicular joint. Both schools of thought can put forward excellent results to support their case. Not all conservatively treated acromioclavicular dislocations do well, and there is a significant morbidity associated with surgery; I suspect the debate will continue for some time. Because the results of conservative treatment are in general so good, it seems only reasonable to treat the majority of patients conservatively. Unfortunately, there are no reliable means of determining which patients will not do well, and hence surgery must always play a part. If a high-risk group could be identified, then acute and early repair would be a rational procedure. However, some feel that they cannot predict which group will do badly and hence treat all dislocations conservatively but accept that some will have to have later reconstructive surgery.
Anatomy and Function
The topography of the acromioclavicular joint varies considerably from subject to subject, but the relationship of the clavicular and the acromial component of the joint is kept remarkably stable throughout its range of movement. The majority of movement taking place in the joint is rotation in the long axis of the clavicle. The conoid and trapezoid ligaments run obliquely from the coracoid to the clavicle in opposing directions and are analogous to the cruciate ligaments of the knee, providing stability throughout the range of movement of the joint.
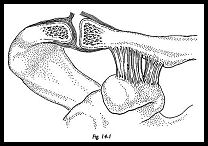
The spectrum of injuries from subluxation to complete dislocation depends on the severity of the trauma. The first structure to disrupt with relatively minor trauma is the superior joint capsule (Fig. 14-1). This is evidenced by very localized acute tenderness related to the superior aspect of the joint. The thickening of the joint capsule ruptures just proximal to the attachment of the intra-articular miniscus.
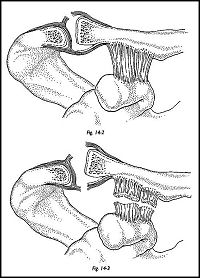
In the complete dislocation, the miniscus always maintains its attachment to the acromion. In a more severe lesion resulting in subluxation, the periosteum is torn away from its attachment to the inferior surface of the clavicle (Fig. 14-2). The evidence for this lies in the frequent radiographic finding of subperiostial new bone formation. With increasing violence, the conoid and trapezoid ligaments, the clavipectoral fascia, and its condensations are torn from a lateral to a medial direction (Fig. 14-3).
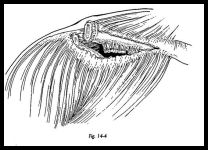
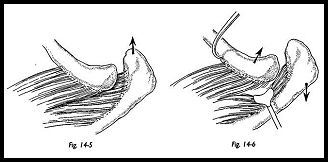
The most severe trauma results in complete dislocation and avulsion of the deltoid from the outer end of the clavicle. A horizontal tear may occur in trapezius between the fibers that are attached to the clavicle and those that are attached to the spine of the scapula (Fig. 14-4). The scapula is now allowed to pull forward, giving the appearance of posterior subluxation of the clavicle (Fig. 14-5). At surgery in late cases, the end of the clavicle can be seen lying beneath the skin and appears to be buttonholed through the trapezius (Fig. 14-6). The acromial fibers of the trapezius prevent passive reduction of the dislocation by direct pressure downward on the clavicle, and these fibers must be divided to allow the joint to be fully reduced.
Classification
Acromioclavicular injuries are a common consequence of all forms of contact sports. The mechanism can be either direct trauma falling onto the point of the shoulder, or an indirect mechanism by forces transmitted along the outstretched arm. Classically, three types of injury have been described by Allman.1
Type I: A simple sprain of the joint with hematoma formation and some partial tearing of the superior capsule but without subluxation.
Type II: Complete capsule tearing with some subluxation of the joint and stripping of the inferior periosteum from the clavicle from lateral to medial.
Type III: Complete dislocation of acromioclavicular joint in association with complete rupture of the coracoclavicular ligaments. This classification has been further modified by Rockwood2:
I. Sprain II. Vertical subluxation
III. Vertical dislocation with intact deltotrapezius aponeurotic envelope
IV. Vertical dislocation with disrupted envelope (subcutaneous) V. Horizontal posterior displacement of clavicle
VI. Inferior displacement (locked under coracoid—very rare)
Indications
Treatment for type I and type II injuries is conservative and noncontroversial. Many and varied operations have been described for the treatment of the complete dislocation. This in itself indicates that probably none of them are entirely satisfactory. A good proportion of people with type III to V injuries returns to a full active sporting life with no symptoms. However, a proportion does not become pain-free, having considerable discomfort in their shoulder girdle, weakness, and inability to take part in sporting activities, particularly throwing. The proportions of these two groups vary widely from series to series. It therefore seems logical to delineate a group of patients who would definitely benefit by early operation. By treating them all aggressively, some would undoubtedly have an unnecessary operation. The list below shows the factors influencing the decision to operate.
For Surgery
- Youth
- Athletic pursuit—particularly throwing sports
- Manual occupation
- Dominant side
- Joint very unstable anteroposteriorly and vertically
- Clavicle lying subcutaneously
- Prefer a scar
- Thin patient
- Reliable enough to take part in postoperative program
Against Surgery
- Age
- Nonathletic
- Sedentary life-style
- Nondominant side
- Joint relatively stable
- Overlying muscle
- Prefer a bump
- Thick subcutaneous fat
- Unreliable patient (alchohol, drugs, mental subnormaliry)
If there is doubt as to whether a patient would definitely benefit from surgery, it is reasonable to treat the patient expectantly, and if he has persistent symptoms, then a late stabilization operation may be done.
Preoperative Investigation
If acromioclavicular injury is suspected, then a specific acromioclavicular joint radiographic view should be requested. An anteroposterior view of the shoulder is not adequate, because (1) the exposure is not correct for the acromioclavicular joint and (2) the film is difficult to interpret because of overlying shadows. A 30-degree cephalic tilt view should be used routinely. An axillary view of the shoulder should also be taken because this will indicate any posterior displacement of the clavicle and may reveal a small fracture that cannot be seen on the standard anteroposterior view.
Stress radiographs are useful to indicate the integrity of the coracoclavicular ligaments. Ten- to fifteen-pound weights are suspended by loops of webbing round the wrists, not held in the hands because this allows total relaxation of the muscles and maximizes the amount of coracoclavicular separation. An anteroposterior view is taken of both joints so that a comparison may be made.
Surgical Treatment for Type III to V Injuries—Acute
In acute dislocation, the aim is to restore completely normal functioning anatomy. All the ruptured structures are repaired, and the joint is temporarily stabilized either by transarticular pin or a coracoacromial screw (Bosworth). Either of these fixations alone without the soft tissue repair rarely gives an adequate functional result.
Technique
A 5-cm strap incision is made 1 cm medial to the acromioclavicular joint. The full extent of the injury is only seen after the deep fascia has been incised in the line of the skin incision.
The intra-articular miniscus nearly always give the appearance of being torn and degenerate in the adult. In cadaveric studies, it has been shown that after the age of 22 the miniscus is almost invariably perforated and shows signs of advanced degenerative change. If possible, the intra-articular miniscus is left in situ. While the joint is still dislocated, sutures are placed in the disruptive coracoclavicular ligaments but left untied until the joint has been reduced and stabilized.
To reduce the joint, some fibers of trapezius may be incised posteriorly to allow the "buttonholed" joint to be reduced. The acromioclavicular joint superior capsule is repaired, and then the joint is held reduced using a bone hook with downward traction. The deltoid with the attached periosteum and capsule is elevated off the anterior edge of the distal 2 cm of the clavicle and is split in the direction of its fibers "until the coracoid process is exposed. The base of the coracoid is palpated in preparation to accept the Bosworth screw. With a finger on the base of the coracoid, the clavicle is drilled, aiming the drill to the base of the coracoid. If the screw is put into the coracoid process itself, this draws the clavicle too far forward and displaces the anatomic alignment of the joint. The aim should be to get the screw as vertical as possible into the base of the coracoid. If a can-ulated Bosworth screw is available, the procedure is easier because a K wire is inserted first, and then the drill and screw are passed over it. The joint is held reduced, and the screw is inserted through the clavicle to the base of the coracoid; the joint should now be stabilized in the anatomic position. The previously placed sutures in the coracoclavicular ligaments may now be tied. Trapezius and deltoid tears are now meticulously repaired, and a subcuticular suture is inserted for skin closure.
Postoperative Management
The patient is placed in a sling for 3 weeks with pendulum exercises only during this time. In 3 weeks, the patient may then actively mobilize the shoulder below 90 degrees abduction or flexion until approximately 8 weeks, when the screw should be removed under a short general anesthetic. Mobilization only below shoulder height is allowed because, above 90 degrees of abduction and flexion, the clavicle undergoes rotation in the coronal plane and hence the screw will certainly loosen but may also break.
Complications
Whatever method of fixation is used, either transacromial pins or the Bosworth screw, both means of fixation must be removed, and hence a second anesthetic is required. If transarticular acromioclavicular pins are used, then these may be removed under local anesthetic. However, I prefer not to use these, because if left either just beneath the skin or through the skin, then local pin site infection is likely. The pins may also migrate and break across the joint. A long-term complication from transarticular pins of course is late degenerative change within the joint. Surprisingly, this appears not to be a great problem, but on first principles, I prefer not to use transarticular pins.
Bosworth screw breakage may occur in the unreliable patient who mobilizes the shoulder powerfully above shoulder height before the pin is removed.
Screw displacement may occur. Some difficulty may be experienced in getting the large thread of the Bosworth screw to enter the drill hole in the base of the coracoid because this must be done by feel. However, the very 'width of the thread of the screw is the strength of the Bosworth screw. A cannulated AO screw is not adequate and can tear out of the coracoid much more easily. If a screw must be used, then it really should be of the Bosworth type, cannulated or uncannulated.
New bone may form at the screw site. This is often seen on postoperative radiographs after removal of the pin but appears not to be a clinical problem.
Late degenerative change in the acromioclavicular joint may occur and is an indication of excision arthroplasty. Excision arthroplasty is not recommended as a prophylactic procedure, because the aim of operation is to restore normal anatomy and hence normal power of throwing in this sporting population. Power of throwing appears to be reduced after excision arthroplasty of the acromioclavicular joint.
Surgical Treatment of Late Unreduced Type III to V Acromioclavicular Joint Dislocation
Copeland and Kessel Method3
A strap incision is made 1 cm medial to the acromioclavicular joint.
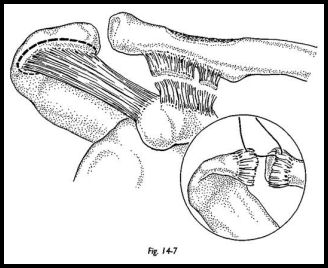
The deltoid is split in the line of its fibers and detached from the outer end of the clavicle, and the acromion is raised on an osteoperiosteal flap at its origin to allow easy suture back onto the acromion and clavicle at the end of the operation (Fig. 14-7). The cora-coacromial ligament is exposed and defined. It is then detached with a large lozenge-shaped fragment of bone from the full width of the undersurface of the acromion, making the bony fragment as long as possible (at least 2 cm). The acromioclavicular joint is exposed, and all obstructing material including the disc remnant is removed.
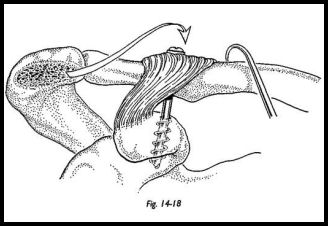
The clavicle is brought forward and downward to its normal anatomic position. The coracoid process is defined by palpation, and its base is visualized directly. The clavicle is then drilled vertically to enter the base of the coracoid process. A small segment of the superior surface of the clavicle around the drill entry site is decorticated (Fig. 14-8). The joint is reduced and held with a bone hook while the coracoacromial ligament is swung across so that its attached segment of bone comes to he on the superior surface of the clavicle. A Bosworth screw is then passed through the flake of bone through the drill hole in the clavicle and into the base of the coracoid. The wound is carefully closed in layers, paying particular attention to the reattachment of the deltoid origin. The direction and mode of fixation of the transposed ligament are such that normal axial rotation of the clavicle causes the new ligament to tighten when the arm is elevated.
Postoperative Management The arm is rested in a sling for 3 weeks, after which active use is encouraged with instructions not to elevate the arm beyond 90 degrees. The screw is removed at 6 to 8 weeks, at which stage a lucent zone will be already evident on the radiograph around the shank of the screw caused by the movement of the clavicle. Following removal of the screw, full movement is regained, and the joint is stable. No long-term disability results from the loss of the coracoacromial ligament.
Complications The main technical difficulty is with getting the correct siting of the lag screw into the base of the coracoid and getting the correct tension on the transferred coracoacromial ligament. The disadvantage is that a second operation is required for screw removal, and new bone formation has been noted around the site when the screw has been removed, although this has not been a clinical problem.
Modified Weaver and Dunn Method
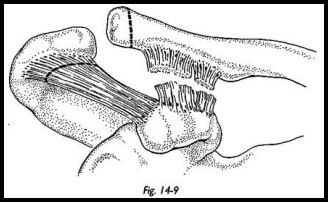
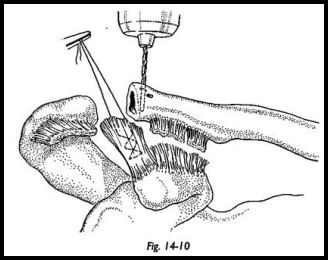
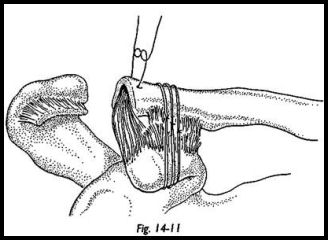
The modified Weaver and Dunn method4 may be indicated in the acute and the late unreduced injury. Originally, a curved incision along the line of the clavicle was described, but the operation is more easily performed through the more cosmetic strap approach. The origin of the deltoid muscle is detached and reflected laterally, exposing the distal part of the clavicle, the coracoid process, and coracoacromial ligament (Fig. 14-9). The acromial end of the coracoacromial ligament is detached, and the ligament is dissected free to the coracoid process. The lateral centimeter of the clavicle is removed in an oblique fashion so that the inferior part of the oblique osteotomy overlies the coracoid process (Fig. 14-10). The clavicle is held in an anatomic position relative to the coracoid, and traction is applied to the coracoacromial ligament. The proper length is selected to maintain the reduction. Number 1 nonabsorbable nylon is placed in the ligament. Two small drill holes are made in the superior cortex of the clavicle, the suture material is passed through them, and the coracoacromial ligament is pulled into the medullary canal of the clavicle, securing the reduction. The repair is reinforced with three double strands of number 2 PDS sutures passed around the clavicle and underneath the coracoid and knotted anteriorly. By the time this suture is resorbed, the repair is sound. The deltoid muscle origin and the trapezius insertion are sutured together, and the wound is closed in the standard fashion (Fig. 14-11).
Postoperative Management The arm is placed in a sling, and pendulum and circumduction exercises are encouraged from the beginning. Because there is no internal fixation at the end of 4 weeks, the patient is allowed a full active use of the shoulder.
Dacron Graft Technique
Indications The Dacron graft technique may be used in the acute or late unreduced injury.
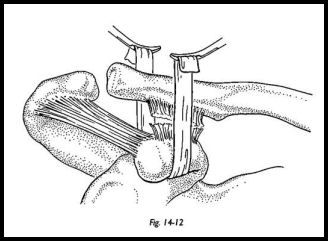
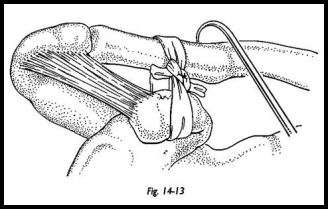
Technique A strap incision is made 1 cm medial to the acromioclavicular joint. The joint is openly reduced, which may require incision of some posterior fibers of trapezius to allow the clavicle to come forward into the reduced position. The deltoid is split and partially removed from the clavicle with an osteoperiosteal flap. The coracoid is palpated through the apex of the split. A long length of Dacron graft is then passed around the undersiirface of the coracoid as near the base as possible using cholecystectomy forceps to grasp the Dacron graft (Fig. 14-12). The graft is then passed around the clavicle again using the holecystectomy forceps. The acromioclavicular joint is now openly reduced, and in late and reduced cases, an excision arthroplasty is made of the joint itself. Once the joint is held reduced using a bone hook, the position is maintained by tying a knot in the Dacron graft under tension. A suture is then used to transfix the knot to prevent this becoming inadvertently untied (Fig. 14-13). The redundant ends of the Dacron graft are now removed close to the knot. The deltoid is reattached meticulously, and the wound is closed with a subcutaneous suture.
Postoperative Management The arm is rested in a sling for 3 weeks with pendulum movement only as pain allows during this time. After 3 weeks, both active and passive mobilizing may be started with the help of the physiotherapist. No contact sports are allowed for 3 months.
Complications Clavicle erosion may be a complication of the Dacron graft technique. When this graft was first used, it was placed through a drill hole horizontally in the clavicle because of the fear of erosion of the graft through the hole of the clavicle. Erosion of the Dacron tape through the inferior surface of the clavicle has been reported. When the graft is passed over the whole of the clavicle, erosion does occur down to approximately one-third the width of the clavicle. During this time, the patient experiences an ache that lasts approximately 2 to 3 months. It seems that the correct tension is then achieved, the erosion stops, and the shoulder becomes symptom free. A complete erosion through the clavicle by Dacron graft has not been reported.
References
- AUman F: Fractures and ligamentous injuries of the clavicle and its articulation. J Bone Joint Surg [Am] 49:774, 1967
- Rockwood CA: Injuries to the acromio-clavicular joint, pp. 680-910. Rockwood Green (eds): In Fractures in Adults. JB Lippincott, Philadelphia, 1984
- Copeland SA, Kessel L: Disruption of the acromio-clavicular joint. Surgical anatomy and biological reconstruction. Injury 208—14, 1980
- Weaver JK, Dunn HK: Treatment of acromio-clavicular injuries. J Bone Joint Surg [Am] 54:1187-93, 19


