Nerves of the Thoracoscapular and Glenohumeral Joints: Anatomy, Cause of Injury, Exposure
Control of the scapula is the basis for function of the glenohumeral joint. Paralysis of the trapezius or serratus anterior disturbs shoulder function and indeed upper limb function to a surprising degree. Bonnel1 showed that one quarter of the nerve fibers in the brachial plexus innervate the shoulder girdle. The spinal accessory, long thoracic, suprascapular, and circumflex nerves are particularly important and are commonly injured.
Some Anatomic Features
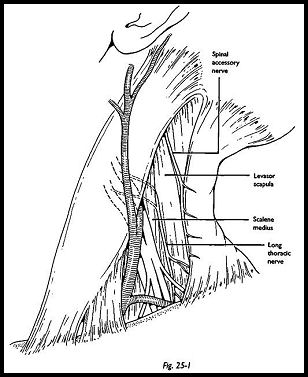
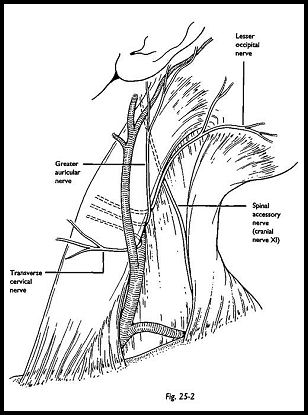
The fibers of the spinal accessory nerve, the external ramus of the 11th cranial nerve, arise from the accessory nucleus, which extends from the 2nd to the 6th cervical segments. It enters the neck through the jugular foramen within the same dural sleeve as the 10th nerve, crossing the retrosryloid space between the mastoid and mandible. The nerve passes deep to the digastric muscle and, usually, deep to the internal jugular vein to enter the sternomastoid between the superficial mastoid head and the deeper occipital head in the upper one third of the muscle. It emerges in the posterior triangle of the neck at the junction of the upper and middle one third of the posterior margin of sternomastoid. There is a constant and useful relation to the sensory branches of the cervical plexus; the transverse cervical, greater auricular, and lesser occipital nerves wind around the sternomastoid muscle just under 1 cm caudad to the accessory. The nerve is about 2 mm in diameter here, containing about 2,000 myelinated nerve fibers (MNF). It lies superficially, crossing the levator scapulae and undulating in fatty tissue and is closely related to the posterocervical lymph nodes. The nerve passes obliquely from the upper to the lateral boundaries of the posterior triangle coming to He deeply to the anterior fold of trapezius. About four branches pass to the upper fibers of that muscle in the posterior triangle. The nerve passes more deeply and inferiorly, lying within the fascia investing the deep surface of trapezius (Fig. 25-1). Sensory branches of the cervical plexus pass superficial to it. The nerve leaves the posterior triangle to pass medially and caudally innervating the middle and lower fibers of trapezius. It is joined, just above the clavicle, by slender branches of C3 and CM. Published work disagrees about the function of this contribution from the cervical plexus, but stimulation of these rami during exposure of the nerve suggests that there are few, if any, efferents to skeletal muscle.
Function
The most important deficit is paralysis of trapezius. Paralysis of the upper fibers leads to drooping of the shoulder girdle and loss of abduction. Paralysis of the middle and lower fibers causes incoordination of scapular movement, which is apparent 'when the shoulder is abducted to about 90 degrees when the scapula wings, and an erroneous diagnosis of serra-tus anterior palsy may be made. At about 90 degrees of abduction, there is loss of control of the scapula, which jerks anteriorly, disturbing die cadence of the shoulder movement. Severe pain is a common complication of injury to the spinal accessory nerve, and there are two possible explanations for this. First, dropping of the shoulder girdle causes traction on the brachial plexus, leading to pain and sensory disturbance. Next is the finding from microneurography that stimulation of muscle nerve fascicles evokes a broadly distributed cramping pain.
The spinal accessory nerve is particularly at risk during surgery in the posterior triangle of the neck. Valtonen and Lilius studied 15 such cases, finding spontaneous recovery in 2 only and persisting severe pain with significant loss of function in 11 of the remaining 13. The nerve is also vulnerable in severe traction lesion of the brachial plexus. Rarely, the nerve is involved in neuralgic amyotrophy and in postirradiation neuritis.
Long Thoracic Nerve
The long thoracic nerve is formed from constant branches arising from the most proximal part of the anterior primary rami of C5 and C6. A branch from C4 is found in about 30 percent of explorations and from C7 in over one half. The rami from C5 and C6 join within the scalenus medius and are joined at the lateral margin of that muscle by the branch from C7. The nerve may be compressed by a fibrous arcade, where it emerges deep to scalenus medius. The nerve, now from 1.5 to 2 mm in diameter, courses laterally to the scalenus medius, lying in a plane posterior to the plexus, to traverse the 1st rib (Fig. 25-2).
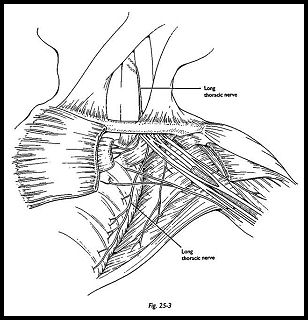
One branch is found constantly just above the superior border of the 1st rib to the first digitation of serratus anterior. The nerve is sinuous as it crosses the 1st and 2nd ribs, and here it is particularly vulnerable in transaxillary operations for excision of rib or cervical sympathectomy. It courses inferiorly and rather posteriorly, invested in fascia overlying serratus anterior, and in close relation to the artery to serratus anterior, a branch of the subscapular trunk (Fig. 25-3). The nerve may be damaged here in operations for axillary clearance or for breast cancer.
The serratus anterior holds the scapula against the chest wall and protracts it. With the trapezius, it provides a stable platform for movements of the upper limb. Although winging of the scapula is the classic sign of paralysis of serratus anterior, this is also seen when the middle and lower fibers of trapezius are paralyzed. When the serratus anterior is paralyzed, the inferior pole of the scapula does not move forward with protraction or flexion of the upper limb; rather it slides medially and cranially. Deep aching pain is common and sometimes severe.
The nerve is most commonly damaged in severe traction lesions of the brachial plexus with preganglionic injury to C5 and C6. Iatrogenic injuries occur in operations in the axilla and breast and during the transaxillary approach to the 1st rib or sympathetic chain. Other iatrogenic injuries have been described from the use of axillary crutches, high plaster jackets, and unpadded shoulder rests. The nerve is commonly afflicted in neuralgic amyotrophy.
Suprascapular Nerve
The suprascapular nerve usually springs from the upper trunk just proximal to the junction of C5 and C6, about 3cm above the clavicle. Rarely, it arises directly from CM. It passes laterally and posteriorly, deep to the amohyoid, to the scapular notch, where it enters the supraspinous fossa deep to the superior transverse scapular ligament. It traverses the fossa deep to the supraspinatus muscle and then winds around the lateral border of the spine of the scapula to enter the intraspinous fossa. The nerve contains between 3 and 4,000 MNFs.
The suprascapular nerve is essential for the function of the glenohumeral joint; without it, abduction and external rotation are lost. Patients with isolated paralysis of deltoid, with a normal suprascapular nerve, and an intact rotator cuff can abduct fully and retain full external rotation.
The nerve is damaged in wounds in the posterior triangle, including those inflicted during operation. The most common injury is traction lesion of the brachial plexus. Coexisting injuries of suprascapular and of circumflex nerve are not uncommon after fractures or dislocations about the shoulder. The nerve may also be involved in neuralgic amyotrophy and entrapment at the suprascapular notch.
Circumflex Nerve
The circumflex nerve is the terminal branch of the posterior cord, separating from the radial nerve just distal to the thoracodorsal nerve, at the level of the coracoid. It arises from the C5 and C6, and it contains between 6 and 7,000 MNFs, which pass through the posterior division of the upper trunk before joining the posterior cord. It lies deep within the axilla, on the subscapularis muscle, and it enters the quadrilateral space with the posterior circumflex vessels. The quadrilateral space is bound above by the subscapularis (anterior) and teres minor (posterior); inferiorly, by teres major; medially, by the long head of biceps; and laterally, by the neck of the humerus. The nerve divides into two branches within this canal; the anterior division continues around the neck of the humerus to innervate the anterior part of the deltoid. The posterior branch is larger, innervating teres minor and the posterior deltoid. One sensory branch, the upper lateral cutaneous nerve of the arm, is a useful landmark where it pierces the deep fascia over the posterior border of deltoid.
The deltoid muscle permits powerful and sustained flexion, abduction, and extension of the shoulder. When the muscle is paralyzed, power of abduction and forward flexion is diminished to about 50 percent of normal; power of extension is reduced to about 25 percent of normal.
Published work suggests that the nerve is not commonly injured and that prognosis for spontaneous recovery in closed injuries is good. Sunderland3 reviewed military series from the World Wars I and II, finding an incidence of just over 1 percent from a total of 15,000 nerve injuries. Seddon4 found good recovery in 27 of 42 cases, mostly caused by fracture dislocations of the shoulder. However, the incidence of rupture of the nerve in fracture dislocation in older patients or after high-energy injuries to the shoulder is higher than these reports suggest. Damage to the suprascapular nerve and to the rotator cuff are important in differential diagnosis. Narakas5 analyzed his very large experience of axillary nerve lesions. In his operated cases, he found isolated lesions of the axillary nerve in 62 and combined injuries of axillary and suprascapular nerves in 27. He also referred to 16 examples of ruptures of the rotator cuff with involvement of axillary or suprascapular nerves.
Circumflex nerve function is lost in closed traction lesions involving the C5 and C6. The nerve is occasionally damaged in operations about the shoulder or in postirradiation neuropathy. The nerve may be involved in neuralgic amyotrophy.
Exposures
In this section, the display within the posterior triangle of the neck with the origins of the long thoracic and the supascapular nerves and the posterior division of the upper trunk are described first. Modified exposures for proximal lesions of the spinal accessory are then described, followed by the exposure of the distal part of the suprascapular nerve. Last, the display of the circumflex nerve below the clavicle is explained.
Supraclavicular Approach to the Posterior Triangle of the Neck
The supraclavicular approach to the posterior triangle of the neck gives access to the spinal nerves and the trunks of the brachial plexus; to the suprascapular nerve proximal to the suprascapular notch; to the long thoracic nerve from its formation to where it traverses the first rib; and with some modification, to the spinal accessory nerve within the triangle. It was developed by George Bonney for exposure of the supraclavicular brachial plexus.
Position of Patient After induction, the patient is put into the semisedentary position with the lower limbs in elevation. The head is secured to a neurosurgical head ring. The injured upper limb, the neck, and the chest are prepared. One of the lower limbs is also prepared in case sural nerve is needed for graft.
Technique The incision is made one finger's breadth above the clavicle, and the platysma is raised with the skin flap. The supraclavicular nerves are preserved (Fig. 25-4). Flaps are elevated to the apex of the posterior triangle above, taking care for the accessory nerve and to show the inferior margin of the clavicle below (Fig. 25-5).
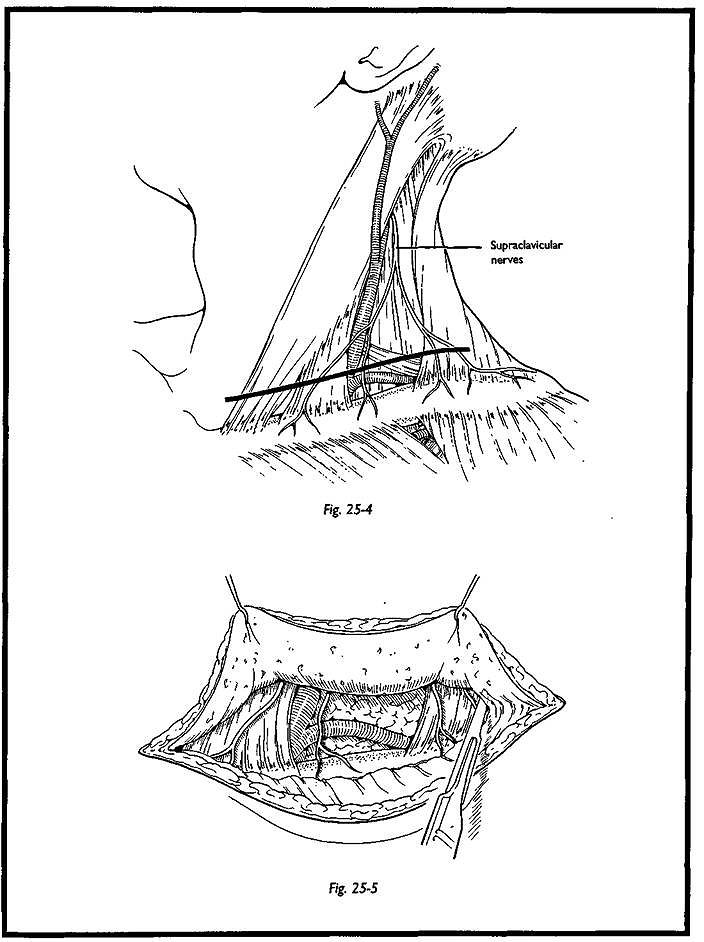
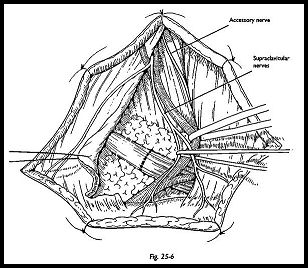
The plane between the sternomastoid and the internal jugular vein is developed, displaying the omohyoid muscle, which is divided between stay sutures and reflected (Fig. 25-6). The fat pad is divided, ligating the transverse cervical vessels, which he deep to it. The phrenic nerve is seen coursing obliquely across the scalenus anterior. This is mobilized and held in a nerve sling.
Following the phrenic nerve cranially brings the surgeon to the C5. Incision of the deep cervical fascia allows display of the C5 and C6 which emerge from under the lateral margin of scalenus anterior, the upper trunk, and the suprascapular nerve. The anterior and posterior divisions of the upper trunk are mobilized and marked by nerve slings.
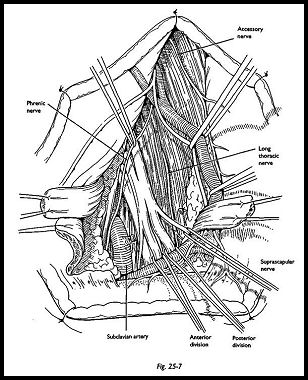
The long thoracic nerve lies lateral and deep to the upper trunk, in the gutter between scalenus medius and scalenus posterior (Fig. 25-7). It is deep to the prevertebral fascia. Tracing the nerve proximally brings one to the margin of scalenus medius, which often forms a fibrous arcade over the nerve trunks. Division of this reveals two rami, one from C6, which is usually larger; another from C5. In about one half of cases, a branch is seen coming down from CM, or a branch coming in from C7. The nerve passes lateral and posterior until just above the 1st rib, where it takes a sinuous course and passes more medial. A branch to the uppermost digitations of the serratus anterior is found here.
Distal Suprascapular Nerve
As Narakas6 points out, suprascapular nerve can be traced from its origin as far as the notch by the supraclavicular approach, but this does not grant useful access to the supraspinous fossa. Adequate display of the nerve as it passes through the notch deep to the superior scapular ligament can be obtained by the approach described by Mansat et al.7 and Hadley et al.8 The exposure can be made as an adjunct to the standard supraclavicular approach in cases of rupture of the nerve. The position and preparation of the patient are as outlined above.
The skin incision is made between the clavicle and the spine of the scapula in the middle of the supraspinatus fossa. The trapezius is split longitudinally to expose the fat pad over the supraspinatus muscle. The upper border of the scapula is palpated. The omohyoid is a useful guide, because it inserts on the medial margin of the notch. The transverse scapular vessels usually pass over the ligament, although they may pass with the nerve beneath it.
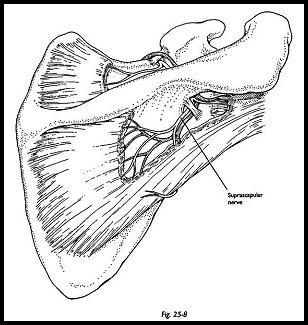
For display of the nerve from the suprascapular notch into the infraspinatus fossa, a posterior approach is necessary (Fig. 25-8). The patient is placed prone. The incision runs from the acromium to the middle of the spine of the scapula. The nerve is seen at the notch by reflecting the trapezius from the spine of the scapula and carefully mobilizing supraspinatus.
Spinal Accessory Nerve at the Apex of the Posterior Triangle
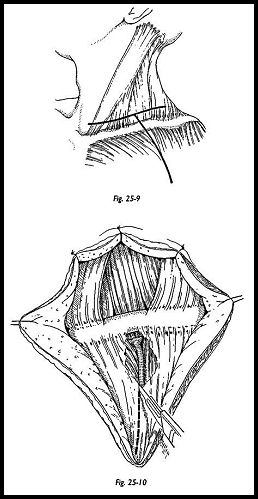
Exposure of the spinal accessory nerve at the apex of the posterior triangle is similar to the standard supraclavicular approach. The incision is dictated by the level of the previous wound from biopsy or from stabbing, the usual cause of damage. A Z-incision or, even better, a V incision raising a flap of skin is recommended so that dissection commences in unscarred tissue. The position of the mastoid and the posterior borders for sternomastoid and anterior border of trapezius should be constantly borne in mind. The key step is identification of the posterior border of sternomastoid and identification of the branches of the cervical plexus, 'which traverse from beneath it to pass anteriorly and cranially. These are in order from below—up, transverse cervical, the greater auricular, and the lesser occipital.
The proximal stump of the accessory nerve is found coursing obliquely downward and posteriorly emerging from within or deep to the sternomastoid muscle no more than 1 cm cranially from the emerging sensory branches of the cervical plexus. Stimulation of the nerve here shows contraction in sternomastoid muscle, confirming one's location.
Distally, the nerve is found in the inner face of trapezius muscle. The superficial fascia is detached from the anterior fold of that muscle and is lifted with fine claw retractors or skin hooks. Terminal branches of the transverse cervical vessels should be ligated, and lateral branches of the supraclavicular plexus should be protected. The nerve is seen bound down to the trapezius by its investing fascia running in a characteristically sinuous fashion. About 2 cm above the clavicle, it is joined by rami from C3 and from CM. Branches are seen passing from the nerve to the upper fibers of the trapezius muscle, and it is essential that these are preserved.
Circumflex, or Axillary, Nerve
The circumflex, or axillary, nerve is most commonly damaged in closed injuries, notably fracture dislocations of the glenohumeral joint. The proximal stump is invariably found anteriorly, but the distal stump may have retracted so that a double exposure with a separate posterior incision may prove necessary. In more complex cases, with injury to the divisions of the brachial plexus from open wounds or from fracture of clavicle, the T-shaped incision is advisable and is combined with osteotomy of the clavicle.
Position of Patient The patient is placed in the semisedentary position, and preparation is as for the supraclavicular approach.
Technique The incision follows the deltopectoral groove, and the cephalic vein is identified and preserved (Fig. 25-9). There is no need to detach deltoid or pectoralis muscles from the clavicle, nor is there any need to interfere with the insertion of pectoralis major onto the humerus (Fig. 25-10).
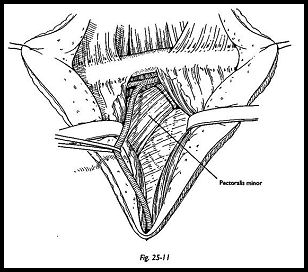
The plane of dissection is deepened to expose the pectoralis minor tendon. Acromiothoracic vessels require ligation. The upper margin of the pectoralis minor is easily definable, and by hooking the finger underneath it, the surgeon can usually readily define the plane between the inferior margin of the muscle and the coracobrachialis (Fig. 25-11).
The pectoralis minor is detached from the corocoid. The medial pectoral nerve enters the muscle medially; the musculocutaneous nerve is not far away.
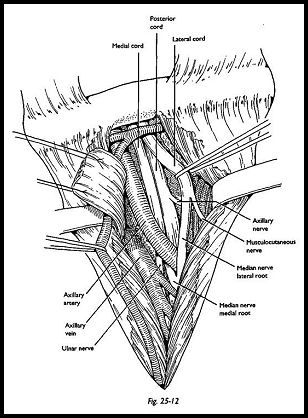
The first structure encountered by the surgeon, gleaming through the fat pad, is the lateral cord of the brachial plexus, and the musculocutaneous and lateral root of the median nerve should be traced. The axillary artery lies behind the lateral cord. The posterior cord in fact lies lateral and deep to the lateral cord and axillary artery.
Malleable retractors are now used to hold the axillary artery and adjacent nerve trunks and to expose the posterior cord as it crosses the subscapularis muscle (Fig. 25-12). The subscapular and thoracodorsal nerves should be seen and protected. In rupture of the circumflex nerve, there will be scarring here. A stimulator is essential, as in all of these exposures, to preserve conducting tissue.
Reflection of coracobrachialis from the tip of coracoid improves exposure of the anterior "door" of the quadrilateral space, and the distal stump of the ruptured circumflex nerve is now seen.
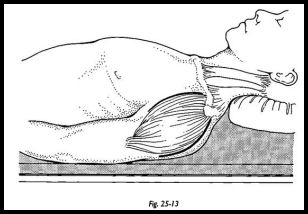
In more severe traction lesions, when the ruptured nerve stumps retract widely, a separate posterior approach is necessary. The incision is made from the proximal insertion of the deltoid muscle to the posterior axillary fold (Fig. 25-13). The upper lateral cutaneous nerve of the arm is the terminal branch of the superficial division of the axillary nerve, and it should be noted following the posterior margin of the deltoid.
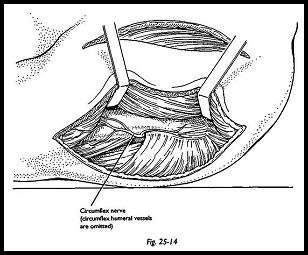
The deltoid is separated from the underlying teres minor, triceps, infraspinatus, and teres major muscles. The circumflex nerve is seen emerging from the quadrilateral space in two divisions together with the circumflex vessels (Fig. 25-14).
Accessory to Suprascapular Transfer
The spinal accessory nerve was transferred in irreparable lesions of the brachial plexus by Kotani et al.9 Allieu10 has great experience of it in reinnervation of the suprascapular nerve, and I am grateful to Professors Allieu and Sedel, who introduced me to this valuable technique.
This operation is particularly useful in irreparable lesions of the suprascapular nerve, almost invariably from pregangUonic injury of C5 and C6. It will not work if the serratus anterior is paralyzed, and the possibility of a second injury to the suprascapular nerve where it passes through the notch or to the rotator cuff should be borne in mind. These problems occur in up to 10 percent of patients with severe closed traction lesions of the brachial plexus.
The nerves are displayed by the standard transverse supraclavicular approach. The suprascapular nerve is traced away from the upper trunk as far proximal as possible, and it is then passed laterally through the fat pad to he adjacent to the spinal accessory nerve. This is sectioned deep in the posterior triangle of the neck, preserving the rami to the upper portion of trapezius. The usual site of section of the nerve is just distal to the end of the branches to C3 and C4. Meticulous hemostasis is necessary, because vessels accompany both nerves, and hematoma at the site of the nerve of repair must be avoided.
References
- Bonnel F: Anatomie du plexus brachial chez le nouveaune et 1'adulte. pp. 3—13. In Alnot JY, Narakas A (eels): Les Paralysies du Plexus Brachiale. Monographies du Groupe d'Etude de la Main. Expansion Scientifique, Paris, 1989
- Valttoeeim EJ, Linus H J: Late sequelae of iatrogenic spinal accessory nerve injury. Acta Chir Scand 140:453-5, 1974
- Souniaieniaiad S: Nerves and Nerve Injuries. 2nd Ed. Churchill Livingstone, Edinburgh, 1978
Sffiddkrat HJ; Surgical Disorders of the Peripheral Nerves. 2nd Ed. Churchill Livingstone, - Mamalkas AO; Neurotization in the treatment of brachial plexus injuries, pp. 1329— 58. In GeHbennian RH (ed): Operative Nerve Repair and Reconstruction. JB Lippincott, PUUe%»nia, 1991
- Nauralkas AO: Paralytic disorders of the shoulder girdle, pp. 112—25. In Tubiana R (ed): The Hand. VoL IV. WB Saunders, Philadelphia, 1993
- Mansat M, Mansat C, Guiraud B: Pathologie de l'epaule et syndromes canalaires. pp. 31—5. In Sarquet R (ed): Syndromes Canalaires du Membre Superieur. Expansion Scientifique, Paris, 1983
- Hadley MN, Sonntag VKH, Pittman HWi Suprascapular nerve entrapment. J Neurosurg 64:843-8,1986
- Kotani PT, Matsuda H, Suzuki T: Triad surgical procedures of nerve transfers to avulsion injuries of the plexus brachialis. Excerpta Med 291:348-50, 1972
- Allieu Y: Les neurotisations par le nerf spinal dans les avulsions du plexus brachial de 1'adulte. pp. 173-9. In Alnot JY, Narakas A (eds): Les Paralysies du Plexus Brachiale. Monographies du Groupe d' Etude de la Main. Expansion Scientifique, Paris, 1989


