Post-operative pain control using a comprehensive programme for day case shoulder surgery
ABSTRACT
Aims: To assess the effectiveness of a peri-operative pain control regimen for day case shoulder surgery, including open and complex procedures.
Methods: A prospective cohort study of all patients undergoing day case shoulder surgery in a single hospital over a one year period, using a comprehensive pain control regimen. The regimen included patient education, interscalene block, analgesics and non-steroidal anti-inflammatories and a cold compression shoulder wrap. All patients were followed up with a telephone call at 24 hours after surgery to assess their pain levels, compliance and any ill effects.
Results: There were 187 patients in the time period, with 90,4% feeling that their pain was well controlled. Fifteen percent experienced moderate and severe pain 24 hours post-operatively. These were limited to five common procedures, with arthroscopic rotator cuff repair and arthroscopic stabilisation being the most common, making up 75% of the reported painful procedures. Only four patients reported severe pain (2%). Two of these took no medications at all. Three of these four patients had 360 degree labral repairs and the other a massive, revision arthroscopic rotator cuff repair.
Conclusion: Post-operative pain following day-case shoulder surgery can be effectively managed with a comprehensive analgesic regimen. This includes open shoulder surgery and complex arthroscopic procedures.
INTRODUCTION
Shoulder surgery has traditionally been considered a painful procedure 1,2 and it had, until relatively recently only been carried out on an in-patient basis, requiring overnight hospital stay. Patients are beginning to accept shoulder surgery as a day-case procedure due to improvements in pain relief. Increasingly it is becoming preferred. The benefits of performing the surgery as a day-case procedure include shorter hospital stay, increased throughput of patients and increased patient satisfaction. The strategies used to improve pain relief and therefore increase acceptability include, most significantly, the use of an interscalene brachial plexus block, supplemented with oral analgesics 2. Supplementary therapies including cold compression can be used to reduce inflammation and promote early healing 3, allowing for early initiation of rehabilitation services, optimising outcome in the longer term.
Despite this progress there are still concerns about the management of post-operative pain in the community and reports suggest that pain remains a problem for a significant proportion of shoulder surgery patients 4. There have also been concerns about the 'rebound pain' which can occur once the interscalene block has worn off.
AIMS
The aims of this study were to assess the post-operative pain of all shoulder procedures in our practice undergoing day-case shoulder surgery (open and arthroscopic), with particular emphasis on the pain once the interscalene block had worn off.
METHODS
A prospective review of 187 patients who underwent shoulder surgery as a day case procedure by a single surgeon over a one year period (from the 10th of November 2008 until the 7th of December 2009) was performed. The analgesic regimen included:
- Patient Education - pre-operative surgical booklets were provided and post-operatively patients were given written and verbal information and instruction on the analgesic regimen by the surgeon, anaesthetist and ward staff.
- A single shot interscalene block with bupivicaine, given prior to surgery
- Diclofenac, codeine phosphate and paracetamol (where tolerated) - patients were instructed to start taking these regularly from about 6 hours after surgery (whilst the block was still working)
- Activewrap (Harvard Healthcare UK) cold compression wrap - commenced 3 hours after surgery and used 15 minutes at a time every two hours.
- Tramadol to be taken for breakthrough pain, if required.
Patients were followed up with a telephone call from the practice surgical practitioner 24 hours post-operatively, allowing sufficient time for the interscalene block to wear off 4. Pain was assessed using a standard visual analogue scale comparative to the Constant Shoulder Score, as shown in Table 1.
Table 1. Visual analogue score for pain:
- 0 = Severe
- 5 = Moderate
- 10 = Mild
- 15 = None
The operations performed are shown in Table 4 (appendix). Although most were arthroscopic procedures, there were 7 open Latarjet shoulder stabilisations (4%), 3 pectoralis major repairs (2%) and 2 shoulder replacements (2%) performed as day-case procedures.
Of the 187 patients, 129 were male and 58 were female. The average age was 43.6 ± 16.1 years, ranging from a minimum of 15 years old to a maximum of 80 years old.
RESULTS
Of the 187 patients 169 considered their pain to be well controlled 24 hours after the operation (table 2). This represents 90.4% of the cohort group (figure 1). The interscalene block had worn off in all cases. None of the patients required an overnight stay or re-admission.
Figure 1. Chart showing proportion of patients satisfied with pain control
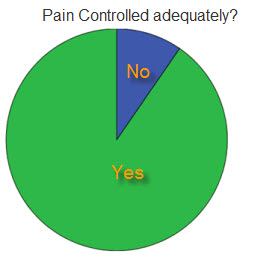
Table 2. Table showing numbers and percentage of patients with adequate pain control
| Pain controlled? | Frequency | Percentage (%) |
| No | 18 | 9.6 |
| Yes | 169 | 90.4 |
| Total | 187 | 100.0 |
A more detailed breakdown of pain reported post-operatively is demonstrated in table 3 and figure 2. The pain was recorded as either absent, mild, moderate or severe and plotted. 85% of patients reported either no painful symptoms at all or only mild pain. Only 2.1%, 4 patients in total were experiencing severe pain 24 hours after the operation.
Figure 2. Breakdown of pain experienced post-operative
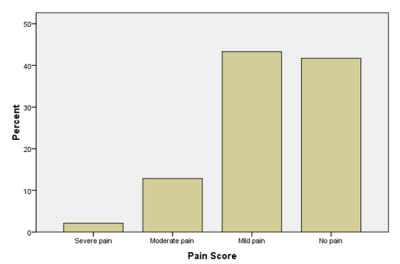
Table 3. Frequency and percentage of pain scores in each patient.
| Pain Score | Frequency | Percentage (%) |
| Severe | 4 | 2.1 |
| Moderate | 24 | 12.8 |
| Mild | 81 | 43.3 |
| None | 78 | 41.7 |
Identifying factors for painful procedures:
There were 28 (15%) cases that reported moderate or severe pain. These were limited to five common procedures only. These were all arthroscopic procedures, with arthroscopic rotator cuff repair and arthroscopic stabilisation being the most common, making up 75% of the reported painful procedures (Table 4).
Only four patients reported severe pain (2%). However, two of these four patients reporting severe pain took no medications at all. Three of the four patients had 360 degree arthroscopic shoulder stabilisation procedures and the other a massive, revision arthroscopic rotator cuff repair.
There was no age or gender discrepancy.
Table 4: Identifying factors for painful procedures
| Operation | Frequency of painful operations | Proportion of painful operations (28) | Proportion of total operations being this procedure (187) |
| ASD & ACJ Excision | 2 | 7.1% | 8.6% |
| Arthroscopic rotator cuff repair | 9 | 32.1% | 12.8% |
| Arthroscopic shoulder stabilisation | 12 | 42.9% | 20.3% |
| Arthroscopic SLAP repair | 3 | 10.7% | 6.4% |
| ASD | 2 | 7.1% | 26.7% |
| Total | 28 | 100.0% |
DISCUSSION
Developments in surgical technique and anaesthetic administration have allowed many shoulder surgeries to be safely and satisfactorily carried out as a day-case procedures. There is still some concern over levels of post-operative pain due to its more challenging management in the community and the after effects of regional anaesthesia. The results of this cohort group demonstrate that 90.4% were pleased with their pain relief, even for open surgery and complex arthroscopic procedures. This level compares favourably with previously published results of shoulder surgery as a day-case procedure which range from 80 to 85% satisfaction 4,5. Our patient compliance was better than previous studies 5, with only two patients not following the post-operative regimen. The reasons for this are likely to be a combination of surgical and anaesthetic factors, as well as thorough patient education. All cases were given an interscalene brachial plexus block. This is a very effective method of reducing pain for the duration of the operation and for around 20-22 hours thereafter 4. There is little doubt that supplemental analgesia is required after the operation. This was anticipated and analgesics were adequately prescribed in the form of co-codamol and diclofenac. Alternative medications including tramadol and ibuprofen were used where codeine, paracetamol and diclofenac were not tolerated due to side effects or contraindications. The anaesthetist performing the plexus blocks was also a specialist in pain management and experience from this field will have contributed to his appreciation of the importance of post and intra-operative pain management. All patients also received instruction on taking their oral medications before the block had worn off in both written and verbal formats from the surgeon, anaesthetist, ward nurses and ward physiotherapist. This allowed patients to understand what they were going through. It empowered them to play their part in optimising their progress through the duration of the recovery period. They were also instructed to apply a cold compression wrap (Activewrap, Harvard Healthcare) for 15 minutes every 2 hours. This works on the principle of maintaining the joint at a lower temperature, decreasing its susceptibility to pain sensation and inflammation 3. Patients using this wrap reported enhanced pain relief and comfort with its application.
CONCLUSION
The results suggest that pain is being effectively managed following day-case shoulder surgery, with a combination of patient education, single interscalene block, codeine, paracetamol, diclofenac and cold compression therapy. This includes open shoulder surgery and complex arthroscopic procedures.
REFERENCES
1. Chung F, Ritchie E ,Su J. Postoperative pain in ambulatory surgery. Anesth Analg 1997 Nov;85(5):986
2. Conroy BP, Fischer RB, Kenter K, et al. Interscalene block for elective shoulder surgery. Orthopaedics 2003; 26: 501-3
3. Singh H, Osbahr DC, Holovacs TF, Cawley PW, Speer KP. The efficacy of continuous cryotherapy on the postoperative shoulder: a prospective, randomized investigation. Journal of Shoulder and Elbow Surgery 2001: 10(6):522-525
4. Wilson AT, Nicholson E, Burton L, Wild C. Analgesia for day-case shoulder surgery. British Journal of Anaesthesia 92(3):414-15, 2004
5. Daruwalla ZJ, Halpenny M, Mullett H. Day case shoulder surgery: satisfactory pain control without regional anaesthesia. A prospective analysis of a perioperative protocol. Ir J Med Sci 2009; 178:57-60
APPENDIX A
Table 4. List of operations performed and relative frequency
Number
Percentage
Arthroscopic Acromioplasty plus ACJ Resection
16
8.6
Arthroscopic Biceps Tenodesis
2
1.1
Arthroscopic Capsular Release of the Shoulder
15
8.0
Arthroscopic Debridement of the Shoulder
6
3.2
Arthroscopic Excision of Calcific Deposit from the Shoulder
1
0.5
Arthroscopic Rotator Cuff Repair of the Shoulder
24
12.8
Arthroscopic Shoulder Stabilisation
38
20.3
Arthroscopic SLAP Repair of the Shoulder
12
6.4
Arthroscopic Subacromial Decompression
50
26.4
Biceps Tenodesis
3
1.6
Latarjet Shoulder Stabilisation (Revision)
6
3.2
Latarjet Shoulder Stabilisation
1
0.5
Reattachment of Pectoralis Major
1
0.5
ACJ Reconstruction
3
1.6
Washout of the Shoulder (Open)
1
0.5
Wound Closure
1
0.5
Hemi-Surface Shoulder Replacement (Uncemented)
2
1.1
ORIF clavicle
2
1.1
Tendon Transfer Around the Shoulder
2
1.1


