MRI of SCR
Post-operative MRI appearances of Superior capsular reconstruction.
By Dr Zeid Al-Ani (Consultant Radiologist) from the Musculoskeletal Ultrasound & injections clinic
www.mskultrasoundinjections.co.uk
Superior capsular reconstruction (SCR) is currently an established surgical technique used to treat patients with large irreparable rotator cuff tears. In this procedure, a graft is attached between the superior glenoid and the greater tuberosity, with the aim of optimising glenohumeral joint function and stability. This article describes the radiological appearances of the intact graft and the various patterns of graft failure.
Usually post-operative imaging includes shoulder radiographs and MRI. Radiographs help to assess the acromiohumeral interval (AHI) and allow for comparison with any previous imaging. Post-operative MRI is not a must, especially in uncomplicated surgeries with good patient outcome but it may detect small areas of partial dehiscence in otherwise asymptomatic patients. MRI is usually performed 6 months after the procedure. Fluid-sensitive sequences (e.g. T2-weighted fat-suppressed sequences) are very important for the assessment of graft integrity. Non-fat-saturated images are also useful to assess the bony details, particularly at the anchors site (Figure 1).
Normal post-operative appearance
On MRI, the intact allograft should demonstrate a homogenous low signal band on T1, T2-weighted and fluid-sensitive sequences, extending from the superior glenoid to the humeral tuberosity (Figure 1 a and b). It should be taut and uniform (measuring at least 3 mm in thickness). The allograft fenestrations can be appreciated as small holes on MRI and should not be mistaken for tears. Increased AHI compared to pre-operative radiographs and concentric position of the humeral head in relation to the glenoid are positive signs indicating good graft function.
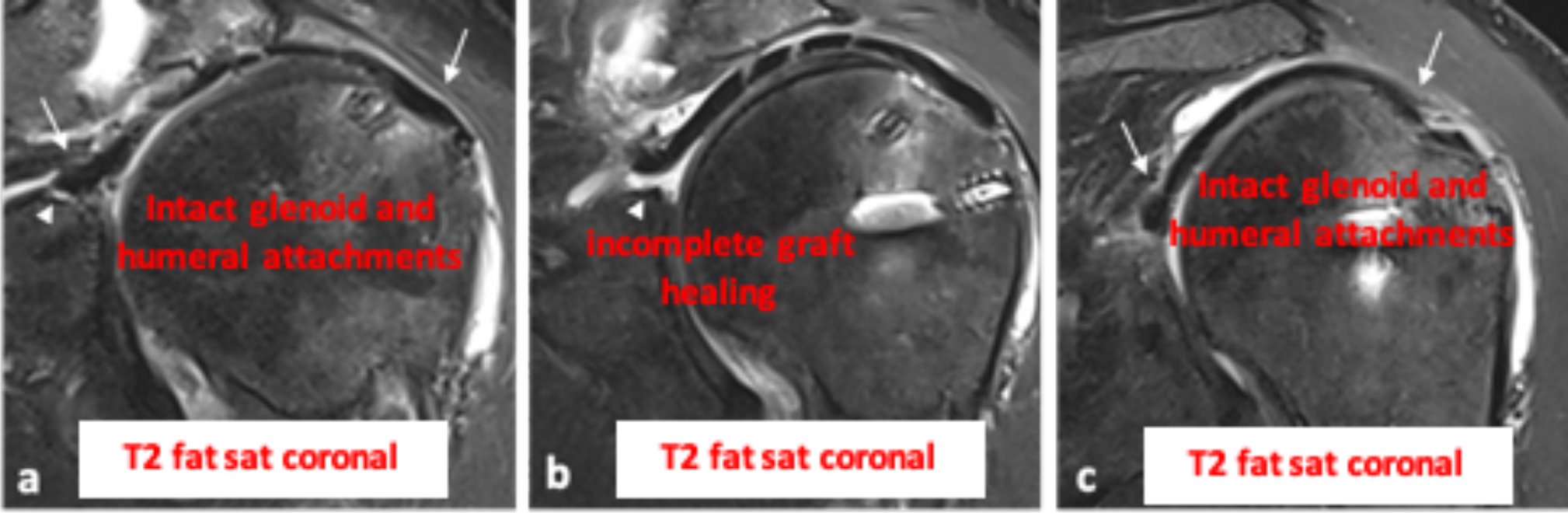
There should be no fluid signal at the humeral or glenoid attachment of the graft, as this would suggest a graft tear. However, the glenoid attachment may demonstrate subtle intermediate signal related to a suture hole, or even sometimes a small, smooth, well-defined cleft of fluid signal (Figure 2). These are acceptable appearances of an intact glenoid attachment, and should not be mistaken for tears. Infrequently, a focal fluid cleft maybe seen completely lifting off the graft from the superior glenoid, with intact appearance at the anterior and posterior graft attachment (Figure 3). This usually indicates a focal area of incomplete graft healing, and in our experience can be seen in asymptomatic patients. Furthermore, the intact graft should be adherent to the infraspinatus tendon posteriorly (Figure 1 c), with no separation or fluid signal at the infraspinatus suture site. The anterior graft edge could be sutured to the rotator interval soft tissues or left free.
Figure 1. Normal appearances
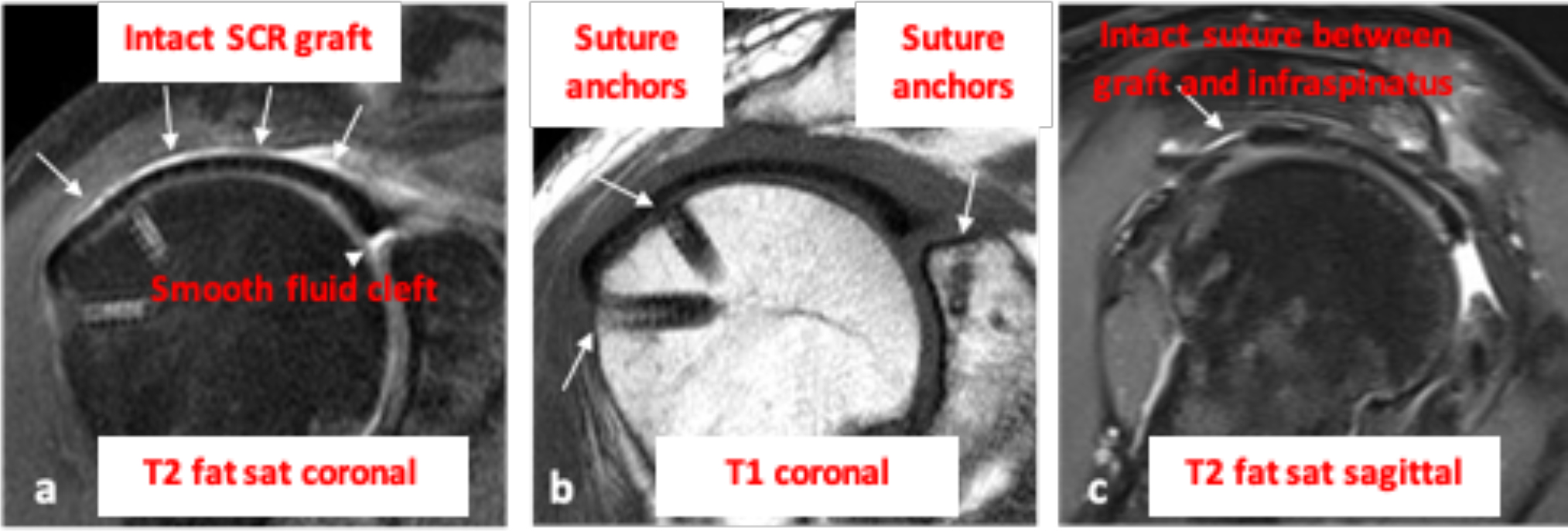
Figure 2. Variation in the appearances of the intact glenoid attachment of SCR graft in different patients.

Figure 3. Intact graft and small area of incomplete graft healing at the mid glenoid attachment (a anterior, b mid and c posterior graft).
Different patterns of graft failure on imaging
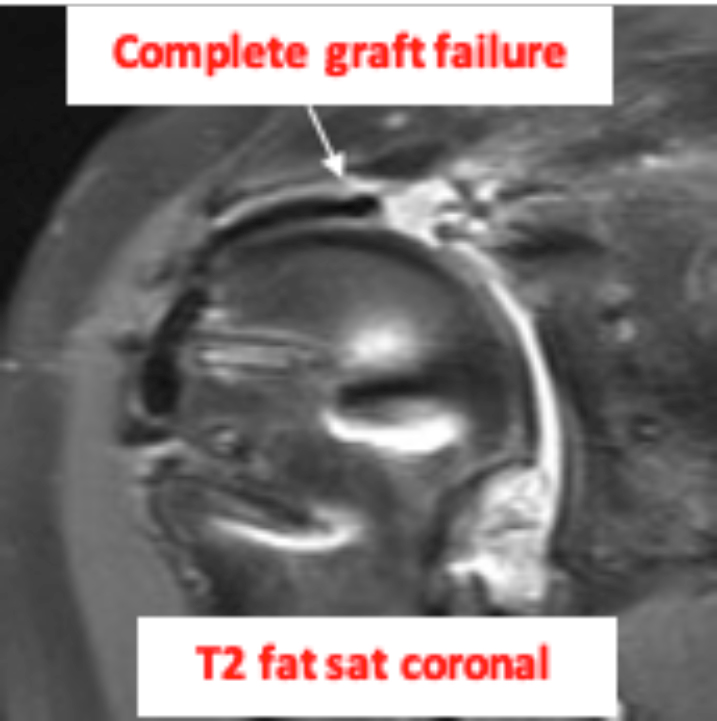
1: Failure at the glenoid attachment
This is demonstrated as fluid signal and discontinuity at the glenoid attachment of the graft. If there is complete tear, then the MRI may demonstrate detachment and retraction of the graft (Figure 4).
Figure 4. Complete SCR graft failure at the glenoid attachment
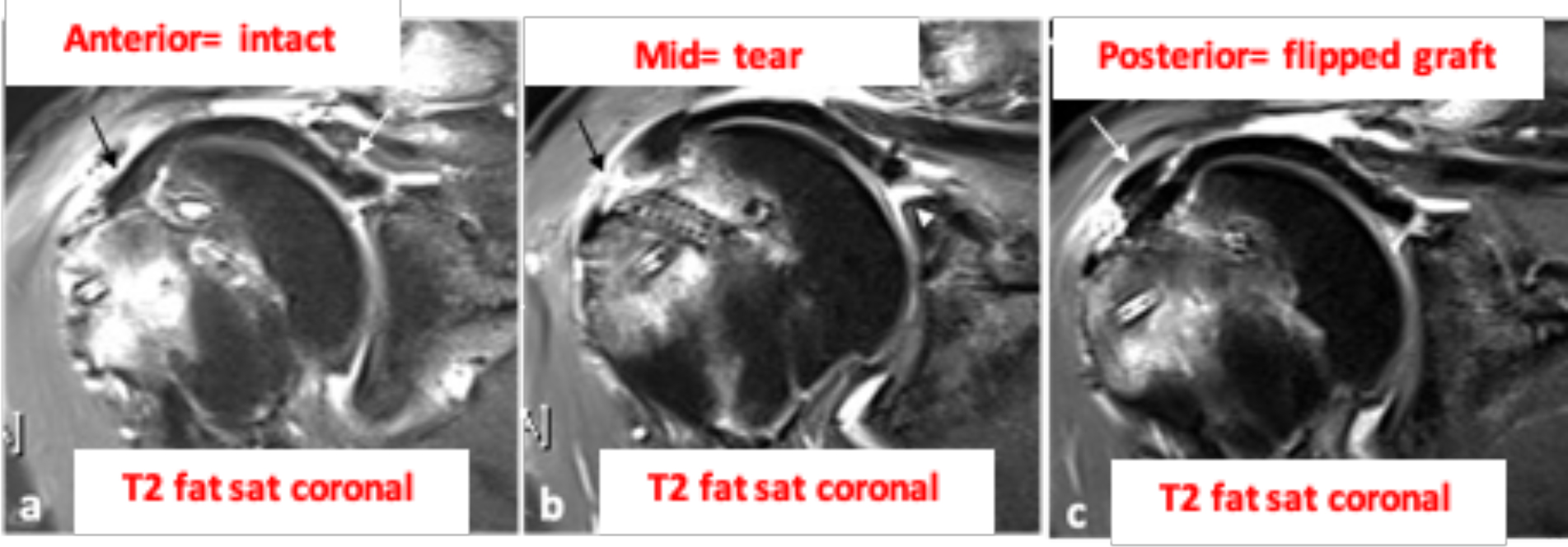
2: Failure at the humeral attachment
Similar to the above, the presence of attenuation, discontinuity or fluid signal at the humeral attachment would indicate graft failure (Figure 5).
Figure 5. Partial tear at the mid humeral attachment with a flipped graft fragment posteriorly.
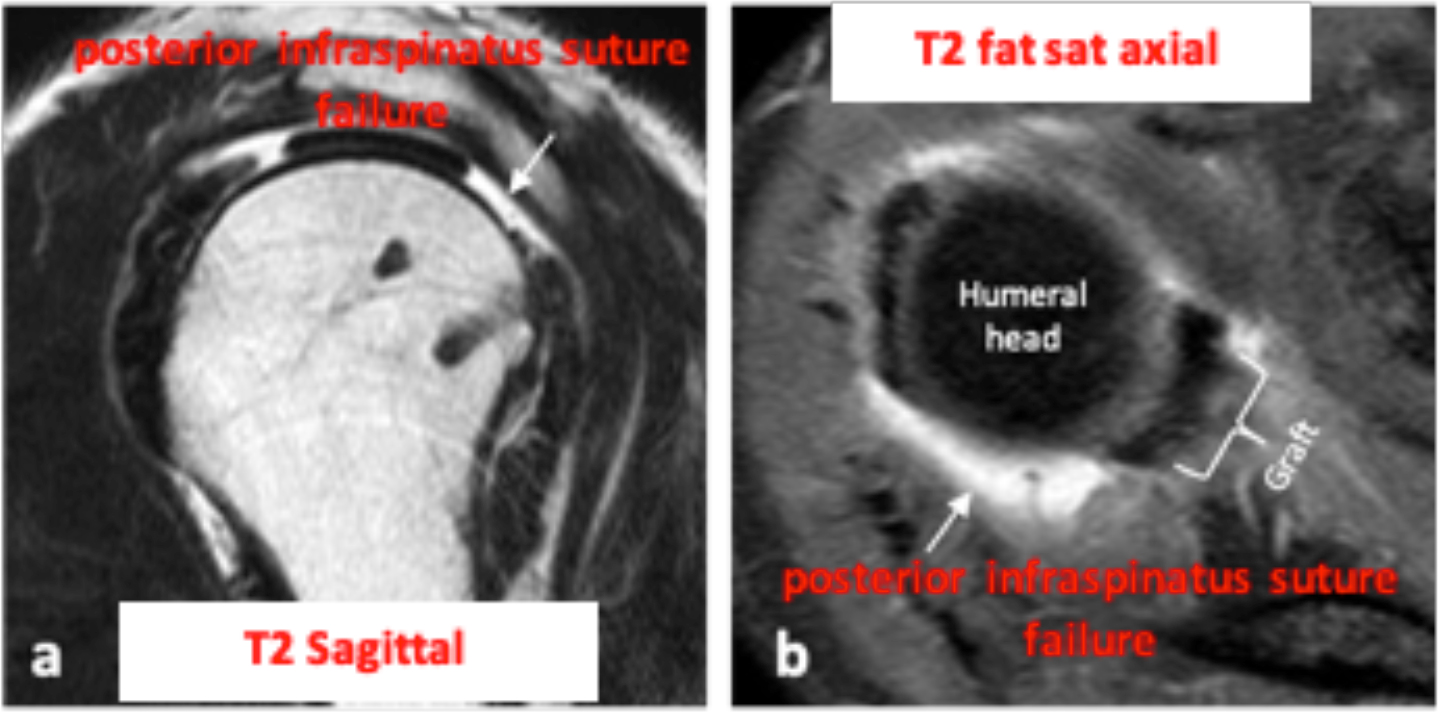
3: Failure at the posterior side-to-side suture with the infraspinatus tendon
Presence of separation and fluid signal between the graft and the posterior infraspinatus tissue would be in keeping with failure of the side-to-side suture with the infraspinatus tendon (Figure 6). Poor posterior remnant tissue is found to be associated with higher rate of re-tear.
Figure 6. Failure at the posterior infraspinatus suture.
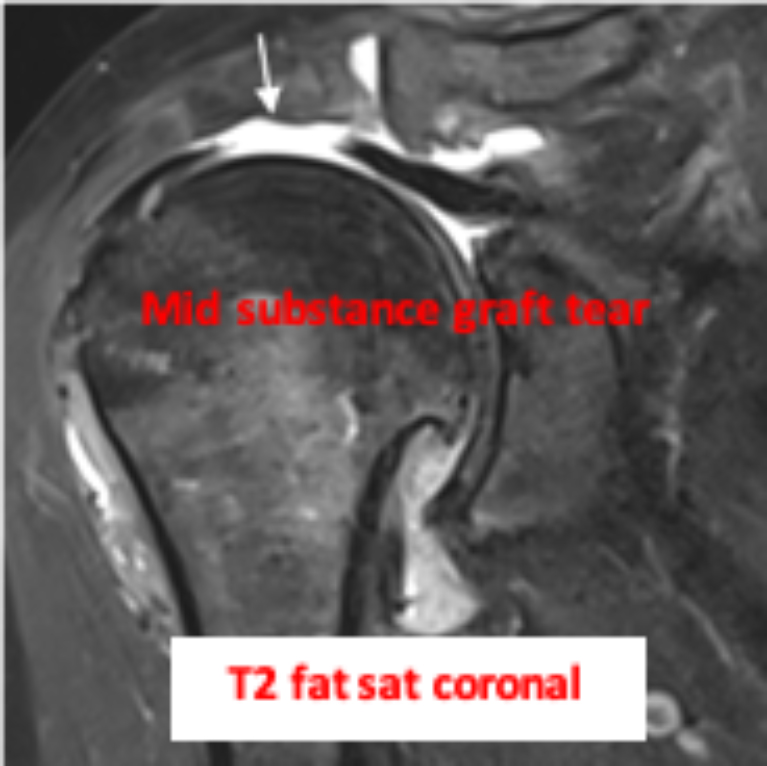
4: Mid substance graft failure
This type of tear is demonstrated as discontinuity and fluid signal within the mid aspect of the graft (Figure 7).
Figure 7. Mid-substance graft failure
- Graft thinning/elongation
The intact SCR graft should demonstrate homogenous low signal and uniform thickness and a well-functioning allograft measures at least 3 mm in thickness. Grafts that measure less than this usually lack adequate strength to prevent superior migration of the humeral head. Therefore, graft thinning is usually associated with graft dysfunction and higher fate of failure.
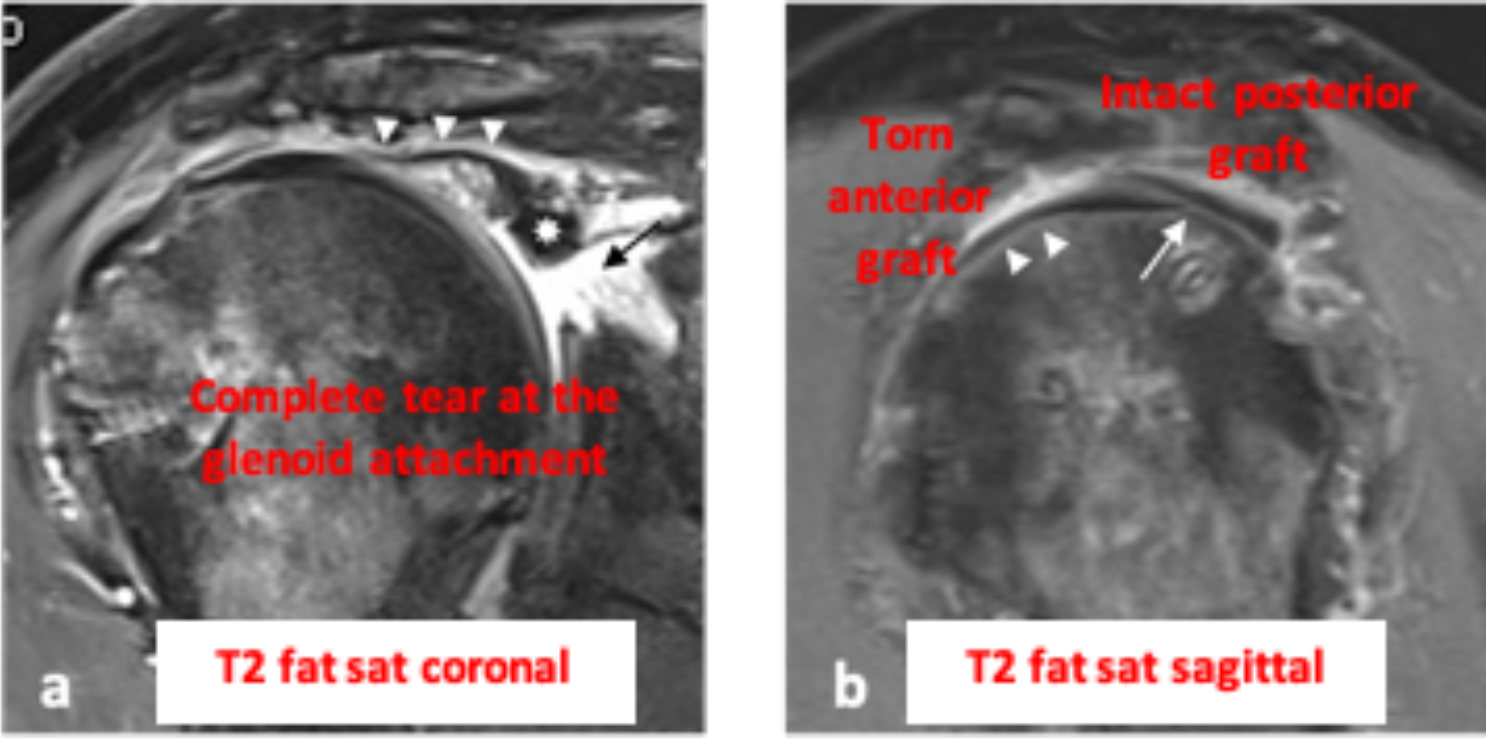
- Complex/multiple tears
Any combination of the patterns described above can happen leading to complex graft failure (Figure 8). These are usually associated with increased graft mobility and can lead to graft displacement.
Figure 6. Complex SCR graft failure
References
- Bernstein JM, Perez JR, Shah HA, Emerson CP, Sanchez PG, Greditzer HGt, et al. MRI of Superior Capsular Reconstruction. Radiographics. 2020; 40(2):454-467.
- Samim M, Walsh P, Gyftopoulos S, Meislin R, Beltran LS. Postoperative MRI of Massive Rotator Cuff Tears. AJR Am J Roentgenol. 2018; 211(1):146-154.
- Denard PJ, Brady PC, Adams CR, Tokish JM, Burkhart SS. Preliminary Results of Arthroscopic Superior Capsule Reconstruction with Dermal Allograft. Arthroscopy. 2018; 34(1):93-99.
- Lee SJ, Min YK. Can inadequate acromiohumeral distance improvement and poor posterior remnant tissue be the predictive factors of re-tear? Preliminary outcomes of arthroscopic superior capsular reconstruction. Knee Surg Sports Traumatol Arthrosc. 2018; 26(7):2205-2213.
- Denard PJ, Brady PC, Adams CR, Tokish JM, Burkhart SS. Preliminary Results of Arthroscopic Superior Capsule Reconstruction with Dermal Allograft. Arthroscopy. 2018; 34(1):93-99.
- Duchman KR, Mickelson DT, Little BA, et al. Graft use in the treatment of large and massive rotator cuff tears: an overview of techniques and modes of failure with MRI correlation. Skeletal Radiol. 2019; 48(1):47-55.


