History
Diagnosis of shoulder disorders depends mainly upon the history. There are often few signs to elicit. Patients will usually complain of either shoulder pain or loss of function. Rarer presentations may include instability, clicking, popping, snapping, a numb or 'dead arm', weakness or stiffness.
There are three key questions that need to be answered:
- Is this true shoulder pain?
- How did the pain start?
- Which movement exacerbates the pain?
of acromioclavicular joint pain (Figure 2.2). True shoulder pain must be differentiated from neck pain, radicular pain and referred pain.
Neck pain originates in the neck and may be referred down to the shoulder, into the interscapular area or up towards the scalp. Root pain may be felt around the shoulder, but originates from the base of the neck and radiates all the way down the arm into the hand. Pain may be referred to the shoulder from diaphragmatic irritation, classically from gallbladder disease to the right shoulder and from the heart to the left shoulder (Figure 2.3).
Is this true shoulder pain?
True shoulder pain is felt at the shoulder and radiates into the upper arm. The patient will describe this in one of two ways. The palm sign describes the patient placing the palm of the unaffected hand over the epaulette area of the painful shoulder and rubbing. This is the usual presentation of glenohumeral or subacromial true shoulder pain (Figure 2.1). The finger sign describes the patient taking the index finger of the opposite hand and pointing to the affected acromioclavicular joint which is pathognomonic
How did the pain start?
The patient may volunteer that the problem started with an injury. If so, a detailed description should be sought:
— When was the injury?
— What happened?
— Was it a soft tissue injury, a fracture or a dislocation?
— What was the position of the arm?
— How much energy was absorbed by the arm?
— How was it managed and by whom?
— Were radiographs taken?
.jpg)

Figure 2.1 The 'palm sign': the patient points to the site of glenohumeral pain by rubbing the shoulder with the palm of the opposite hand.
Figure 2.2 The finger sign': the patient points to the acromioclavicular joint pain with one finger directly on the affected joint.
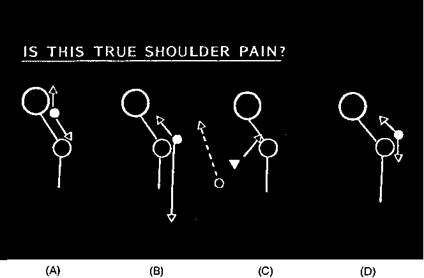
Figure 2.3 Types of shoulder pain. From left to right: neck pain starts at the neck and radiates to the shoulder and up into the scalp (A). Root pain may be maximal at the shoulder but radiates down the length of the arm to the hand (B). Pain may be referred to the shoulder, classically from the diaphragm and gallbladder to the right shoulder and from the heart to the left shoulder (C). True glenohumeral joint pain may radiate both down the arm and also, to a lesser extent, up into the neck (D).
To what degree did it recover and in what time period? Which movement exacerbates the pain?
If there was no injury:
— Did the pain come on suddenly or insidiously?
— Is there any history of arthritis in any other joint?
— Has the patient had any recent infections?
— Is the patient generally well?
Pain at rest is a worrying symptom. The patient may be systemically unwell or well. If the patient is systemically unwell, then sepsis or polymyalgia rheumatica should be considered. If the patient is well, then the pain is usually due to early arthritis of the shoulder or a developing capsulitis (frozen shoulder). These patients will usually have a stiff shoulder on examination with limitation of external rotation and limited flexion and abduction. They may have a terminal painful arc such that elevation is restricted to 100 degrees, with a painful arc between 70 and 100 degrees.
Pain on movement denotes a painful arc of which there are four types: terminal, of the stiff shoulder (capsulitis arc, as above); subacromial; acromioclavicular; and composite (Figure 2.4).
The subacromial painful arc produces an arc of pain which comes on at approximately 70 degrees of elevation or abduction and eases off at approximately 130 degrees to top elevation. This usually indicates pain arising from subacromial impingement. A trap for the unwary is that subacromial impingement in a patient under the age of 40 is often a sign of shoulder instability causing functional impingement (see Chapters 8 and 9). Proof of the pain originating in the subacromial region can be demonstrated by the impingement test (see below).
The acromioclavicular painful arc produces an arc of pain at the extreme of shoulder elevation, between 140 and 170 degrees. This usually denotes pain arising from the acromioclavicular joint which can be blocked by the injection of local anaesthetic.
The composite painful arc has a near normal range of shoulder elevation, but a painful arc from 70 degrees to the top of elevation, a fairly common situation. It occurs in patients with dual pathologies, such as acromioclavicular pain and subacromial impingement.
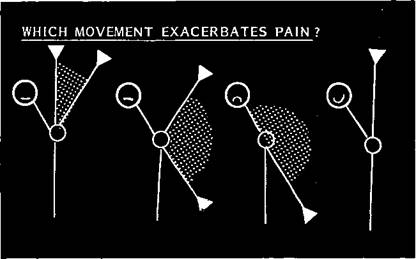
Figure 2.4 Which movement exacerbates the pain? From left to right: the high painful arc of acromioclavicular joint disease, the common painful arc of impingement, the stiff painful shoulder (frozen shoulder). Some people may have shoulder pain which is not exacerbated by movement.
Severity of pain and function
Once the three key questions have been answered, the surgeon will gain further insight by enquiring into the severity of the pain, its frequency, pain at night (a particular feature of shoulder pain) and functional loss. The patient attending the shoulder clinic may be asked to complete a self-assessment sheet while waiting to see the surgeon (Figure 2.5). This scores pain from nil to severe (1-5), the frequency of pain from none to constant rest pain (1-5), and pain at night from none to unable to sleep every night (1-5). Thus a patient scoring 5s all the way is in severe trouble and is asked to complete a form on each attendance giving an objective assessment of improvement. The patient also marks on the form which movements make the pain worse and any change since the last attendance (better or worse). The surgeon also scores the pain and notes analgesic consumption on a separate assessment sheet (Figure 2.6).
Functional loss is as vital to the patient as pain and this is also scored on the self-assessment form. Reach is assessed to shoulder blades, shelves above head, hair, waist, back of neck, base of spine and opposite axilla. Finally, loss of work, sport and sleep are scored. Functional loss has been used by many surgeons who have tried to devise shoulder scoring systems. The Mayo score includes driving, dressing, sleeping and overhead working; the Neer score emphasizes perineal care, dressing, carrying, throwing and lifting. The Lysholm score is used in Sweden and the Constant score in the United Kingdom. Functional assessment based on the Neer score is included in the computerized diagnosis program used by Johnson, which is a 42-page document detailing medical history, shoulder history, shoulder examination, investigations, and shoulder surgery.
It is vital to know the patient's exact occupation and hand dominance and how this is affected by the shoulder pain, if this has not already been elicited at the start of the interview.
Specific questions
Specific questions may now be asked such as the presence of joint stiffness, clicking, popping or snapping sensations and jamming of the joint.
The patient should also be asked whether the joint has ever been dislocated. If so, the initial event should be documented, together with the number of recurrences, the direction of dislocation, the ease of reduction and any feelings of instability without the joint actually dislocating.


