Injection Around the Shoulder
Injection of the Subacromial Bursa
Indications
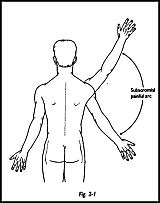
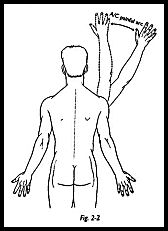
Impingement Injection of the subacromial bursa is of the greatest importance in identifying the source of shoulder pain. Approximately 40 percent of patients attending a shoulder clinic with the primary diagnosis of pain will have pain arising from the subacromial area (Fig. 2-1). The painful arc syndrome is not a diagnosis but is a clinical sign; a painful arc of motion between 60 and 120 degrees of abduction indicates that the pain may well be arising from the subacromial region. Pain arising from a higher arc of abduction between 120 and 180 degrees indicates pain arising from the acromioclavicular j oint (Fig. 2-2). Kessel and Watson,1 with elegant inj ection studies of radiopaque dye placed differentially into the tendons of the rotator cuff, have shown radiographically that the central arc of pain is associated with impingement of the cuff. However, -when the shoulder is elevated in the high arc between 120 and 180 degrees, the clavicle must undergo an obligatory rotation in the coronal plane and cause rotation at the acromioclavicular joint; hence, any pain arising here will be maximum during this range of rotation. Neer2 described a similar injection test in which the subacromial painful arc of motion was abolished by injection of the subacromial bursa with 10 cc of xylocaine. If the central painful arc (60 to 120 degrees) is abolished by this maneuver, then this indicates pain arising from the rotator cuff area and impinging under the coracoacromial arch. Some prefer to identify the site of impingement but within the rotator cuff by injecting the tender spot locally actually into the tendon itself with local anesthetic. I have found the impingement test described by Neer to be clinically the most useful in which the bursa is filled with 10 cc of local anesthetic. If the pain is abolished, then this answers the question "Is the pain arising in the subacromial region?"
Therapeutic If the diagnosis of impingement of the rotator cuff has been made, then part of conservative therapy may well include injection of steroid into the subacromial bursa. Opinion varies as to the amount and frequency that it is safe to inject this site. A reasonable approach is no more than one injection every 3 weeks, with a maximum of three injections during any course of treatment. Injection is most useful in stage 2 impingement (see Ch. 4 for staging of impingement). In stage 1, the symptoms almost certainly will settle with rest alone, and hence the dangers of injection can be avoided. In stage 3, changes may be too severe to gain any benefit from injection alone. There may be three possible results from therapeutic injection of the subacromial bursa:
- Complete resolution of symptoms permanently, in which case, nothing further need be done apart from general advice to the patient to prevent further occurrence
- No effect at all, in 'which case the diagnosis was 'wrong or the injection was incorrectly placed
- Partial resolution of symptoms
Partial resolution of symptoms may be taken to mean (1) complete resolution of symptoms but only for a short time 'with complete return of symptoms, or (2) improvement in symptoms, but not complete resolution. In both these situations, it is known that the injection has been correctly sited and that further injection may well be helpful. It may be thought that impingement has two pathologic results. (1) Pure inflammatory change leading to localized edema, -which if left unresolved for too long, will lead to (2) fibrosis. Local steroid injection will certainly reduce the inflammatory swelling to allow the rotator cuff to slip under the coracoacromial arch, but it will do little for scarring. Hence, if a mixed injection of local anesthetic plus steroid gives only relief for the length of time required for the local anesthetic to -wear off, then it is known that the injection has been correctly sited but that the majority of the symptoms are arising from fibrosis, which is unresponsive to the steroid, and hence further injection would not be helpful. However, if the symptoms are completely reheved for longer than the effect of the local anesthetic, then the inflammatory swelling must be a large part of the symptoms, and hence repeated injection may well be worthwhile.
Bursagram The injection of radiopaque dye followed by air may be required for double-contrast bursography.
Aspiration of Subacromial Bursa Aspiration of the subacromial bursa may be required to alleviate symptoms in the rheumatoid, but is usually combined with steroid injection, or may also be helpful in the infected bursa to aspirate fluid for culture.
Injection/Aspiration of Calcific Deposit In acute calcific suprasprinatus tendonitis, subacromial bursa injection can be extremely therapeutic. It can certainly relieve the pain from this disabling condition, and if done under radiographic control, aspiration may well be possible. However, this is not easily done. More often in the acute phase, if the subacromial bursa is injected with local anesthetic alone, this allows manipulation of the shoulder, which bursts the calcific deposit and can relieve the symptoms in this way.
Technique
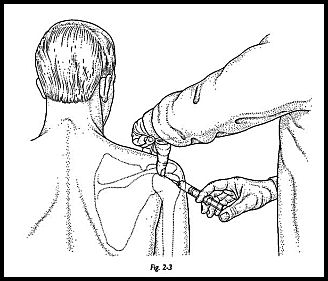
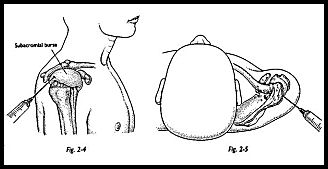
The patient sits in a chair with the arm resting in the lap. A skin antiseptic preparation and a nontouch sterile technique are used. The thumb is used to palpate the angle of the acromion (Fig. 2-3). The point of injection is 1 cm anterolateral to this point. The needle is directed 45 degrees upward and inward. A 23-gauge needle is used (Fig. 2-4). If a finer needle than this is used, then there is no feeling of "give" as the needle enters the bursa. Any wider bore needle is unnecessarily painful (Fig. 2-5). It is recommended that the bursa is entered with local anesthetic alone, and if a steroid is to be used also, then a mixture of the local anesthetic plus steroid be given once the bursa has been entered.
Postinjection Management
If the injection has been purely local anesthetic for diagnostic purposes, no special postoperative instructions are given, apart from warning the patient that the shoulder may well be uncomfortable when the local anesthetic wears off.
Pain In approximately 15 to 20 percent of patients undergoing a mixture of steroid and local anesthetic injection of a subacromial bursa, pain may well be exacerbated when the local anesthetic wears off. This may last for 48 hours, but as long as the patient is told that this may be so, then fear is allayed and anxiety kept to a minimum. If necessary, a sling can be used during this painful period. The majority, however, do not experience increased pain following injection and can be told to use the shoulder -within normal pain-free limits. They are warned against repetitive use of the arm above shoulder height, or anything that caused the pain before the injection, to allow the inflammatory change to resolve.
Subcutaneous Lipodystrophy Subcutaneous lipodystrophy can occur with any inadvertent subcutaneous steroid injection at any site but is particularly ugly around the shoulder in a young female patient. Hence, any subcutaneous injection must be avoided, and steroid should only be injected into the bursa itself.
Weakening of Tendon/Muscle and Rotator Cuff Rupture Weakening of tendon/ muscle is always the major concern when injecting in this region. There is no doubt that steroid into tendon and muscle significantly weakens collagen fibers and can precipitate the rotator cuff rupture. The chance of this happening when the injection is made into the bursa itself rather than into a muscle or tendon is very much less but is always a possibility. If the above precautions regarding frequency and time interval are followed, then this is kept to a minimum. Should a rupture occur following an injection, then it is fair to assume that the rotator cuff was in a poor and weakened condition significantly before the injection, such that the injection was "the straw that broke the camel's back."
References
- Kessel L, Watson M: The painful arc syndrome. Clinical classification and guide to management. J Bone Joint Surg [Br] 59:166
- Neer CS: Impingement lesions. Clin Orthop 173:70, 1983


