Stabilization of the Shoulder
Shoulder Instability
Dislocation occurs at the glenohumeral joint more frequently than any other joint. The multiplicity of surgical procedures available is testament to the fact that none can be universally successful. In any large series dealing with shoulder dislocation, by far the largest proportion of patients 'will be those suffering from traumatic anterior dislocation. The results can depend more on how well this particular group has been selected than the type of surgery undertaken. Hence, in comparison of results from different series, the diagnostic criteria for including patients need to be directly comparable.
In the diagnosis of instability, methods have been improving such that more appropriate surgery can be applied and better results achieved. It is only with the advent of more sophisticated methods of investigation (arthroscopy, double-contrast arthroto-mography, magnetic resonance imaging) that the pathology can be more accurately identified. Until recently, treatment has been based on the perceived pathologic anatomy as viewed only by the naked eye and by plain radiograph. This explains the different fashions in stabilization procedures and the geographic variations.
The terminology surrounding instability of the glenohumeral joint can become quite complex. Therefore, it is probably better to stay with the simple etiologic classification proposed by Neer et al.1 of atraumatic, traumatic, and acquired. Then apply this to the direction—anterior, posterior, inferior, and multidirectional. Even with these simplistic groupings, there is often an element of each in individual groupings, and the edges of the groupings are blurred. Age is the factor that has the greatest influence on recurrence, such that the incidence of recurrence is so high following a first dislocation between the ages of 17 and 23 that some surgeons are prepared to perform a stabilization procedure on the evidence of one dislocation alone in this age group. The incidence is only unacceptably high if contact sports are continued. Some patients in this age group may be happy to give up sport if the alternative is surgery. A large proportion give up contact sports after school and college years and are happy to accept less demanding sports. They must be given the opportunity to arrive at this decision and not automatically offered surgery.
When thinking about the different types of instability, it is useful to imagine the two opposite ends of the spectrum of patients that present with symptoms of instability. JVLatsen has usefully described the opposite ends of the spectrum with two acronyms, TUBS and AMBRI. The TUBS end of the spectrum is the most frequent type of anteroinferior dislocation, that is, that sustained by violent injury in abduction external rotation often associated with a contact sport. The acronym stands for traumatic, unidirectional, Bankart lesion, and the treatment is surgical. In other words, this was a previously normal shoulder with a completely normal opposite shoulder until it was subjected to such violence that the normal structure was completely disrupted to allow dislocation. The other end of the spectrum is atraumatic, multidirectional, bilateral, treated by rehabilitation (AMBRI), but if conservative treatment fails, then treatment should be by inferior capsular shift. In other words, instability at this end of the spectrum is usually in an already con-genitally lax shoulder, and minimum trauma may have induced an unstable situation. This may have been acquired by no single major event but by repetitive microtrauma of repetitive stretching, such as throwing, serving at tennis, or backstroke swimming. In this group, the joint may not be truly dislocated but may just give symptoms of instability and may present as momentary subluxation (dead arm syndrome) or as impingement pain secondary to instability. This group is commonly treated by rest, particularly with a night sling, and a rehabilitation strengthening program; if none of this is adequate, then the whole joint capsule needs to be tightened. The direction of maximal instability needs to be determined, and care should be taken not to tighten too much in any one direction, because it may induce instability in the opposite direction.
Preoperative Investigation
A careful clinical history provides the diagnosis in the majority of cases 'with true traumatic dislocation, often present on radiographs from a previous dislocation that demonstrates the direction of dislocation. The apprehension sign is most valuable. On gross testing, it can, of course, distinguish fairly easily between anterior and posterior instability with external and internal rotation, respectively. However, once it has been decided that anterior instability, for example, is present, the position of apprehension according to the degree of abduction can give a clue to the site of capsular damage. Turkel et al. have shown in very elegant anatomic studies that, in 90 degrees of abduction with external rotation, only the inferior glenohumeral ligament prevents anterior subluxation of the humeral head; subscapularis in this position has already rolled over the head of the humerus.2 Hence, apprehension in midrange abduction with external rotation indicates an anteroinferior instability, -whereas apprehension in high elevation and external rotation suggests a pure inferior dislocation. Apprehension with the arm by the side in forced external rotation indicates a pure anterior dislocation requiring pure anterior stabilization. The degree of joint laxity must be assessed, and the opposite shoulder of course must be examined.
If there is still doubt as to the diagnosis folio-wing clinical examination, history, and plain radiography, then more sophisticated investigations are required. Special plain radiograph views may be obtained to determine the size of the Hill-Sachs lesion (hatchet deformity; these views are discussed in Ch. 12).
Computed tomography (CT) in association with double-contrast arthrography has been most useful in giving preoperative information concerning the direction of instability and intra-articular damage in the difficult instability often associated with highspeed trauma. Magnetic resonance imaging has been found to be less useful than dou-bl e-contrast CT in assessing stability. Arthroscopy shows us that the anterior labrum is a functional extension of the glenohumeral complex.
O'Brien et al. describe the glenohumeral ligament as a hammock on which the humeral head rests.3 The Bankart lesion can be likened to sectioning one of the supporting ropes of the hammock, causing the head to fall forward. This avulsion of the anterior part of the inferior glenohumeral ligament can be assessed arthroscopically. Some do not show this avulsion, and the anterior capsule is noted to be scarred and lax. The anterior glenoid may be seen to be round and eburnated with thinning of the anterior labrum indicating an anterior subluxation. At arthroscopy, the humeral head may also be visualized, and the Hill-Sachs lesion identified and an assessment made of its size. Because arthroscopy is usually performed under general anesthesia, this can usually be done before any stabilization procedure and can also be done at the same time as examination under anesthetic (EUA). EUA (see p. 92) is thought to be an essential prerequisite to assessing the unstable shoulder before surgery. Even when the patient has a known multidirectional instability previously clinically determined, EUA can help determine the direction of maximal instability.
The most difficult group of all to treat are the so-called atraumatic voluntary, or habitual dislocators. It is often said these have some psychiatric abnormality, and when tested, they present a normal psychiatric profile. There is no doubt that this is related to age and both emotional and physical maturity. The patients usually present between 14 and 20 years, and the majority usually self-stabilize with age without resort to surgery. However, some do not, and at the present time are usually beyond surgical help apart from specific indications. The most valuable physical sign when examining these patients occurs during attempts to reduce the shoulder -while palpating the resistance of the patient's muscles. These patients make an effort to hold the humerus out of joint. This is the so-called resistance to reduction sign. It needs to be demonstrated to these patients that they are pushing their shoulder out of joint, and it is certainly not loose and falling out of joint. They are told that the shoulder is located while they are asleep, and it is only when they combine certain muscle actions that they push the shoulder out of joint, therefore their muscles must be re-educated not to do this particular action. Biofeedback therapy offers one way of demonstrating this to the patients. Interestingly, long-term follow-up study of this group of patients fails to show any incidence of late degenerative change despite recurrent dislocation over many years.
Examination Under Anesthesia
Indications
EUA should be done before any stabilization procedure. It is often said that it is not a useful procedure, as instability of the shoulder is a dynamic abnormality and EUA can test only the static structures. This is certainly true, but any dynamic abnormality will only allow the shoulder to go as far as static restraints allow. If the examination is carried out in a systematic and careful manner, then other more expensive and sophisticated investigations may be rendered unnecessary. In unidirectional instability, the exact direction of the instability may be determined. In multidirectional instability, the degree of instability can be assessed and the direction of major instability confirmed.
Technique
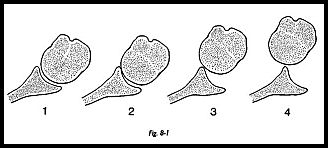
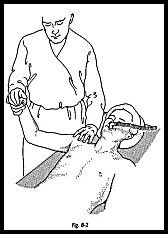
The suspected abnormal side must always be compared with the normal side. It is extremely difficult to define the normal shoulder but very useful to delineate the difference between the symptomatic and asymptomatic side. Under anesthesia, almost any shoulder can be made to sublux. Hence, it is important to develop with experience a scoring system that can be used to chart the comparison between the two shoulders (Fig. 8-1). The patient is placed supine under general anesthetic, and both shoulders are exposed. To examine the right shoulder, the examiner stands at the head of the table and grasps the shoulder with the left hand, such that the thumb is on the posterior surface of the shoulder and the middle finger on the anterior surface (Fig. 8-2). In this way an anteriorly directed and posteriorly directed translocation force may be applied. The right hand grasps the patient's wrist, then the shoulder is tested in different positions of rotation and abduction.
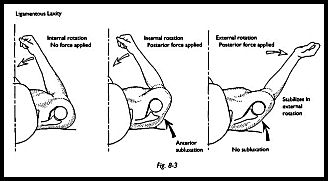
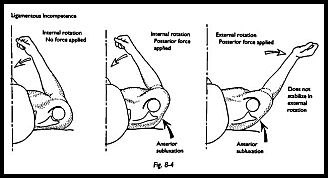
To test for anterior instability, an attempt is made to anteriorly sublux the shoulder with the shoulder in internal rotation and 20 degrees of abduction (Figs. 8-3 and 8-4). Almost invariably, this can be achieved either partially or totally with the patient under anesthesia. A note is made of the degree of translocation. In the same degree of abduction but with full external rotation, the same posterior force is applied. Three results are possible:
- The complete degree of translocation has been abolished. This indicates that the anterior structures are entirely competent, and by putting these on the stretch, the shoulder is stabilized.
- Some degree of translocation is retained but not as much as in internal rotation. This indicates some degree of ligamentus laxity, and if it is the same as the opposite asymptomatic side, it must be considered normal.
- The same degree of translocation is demonstrated as in internal rotation. This indicates that the anterior restraining structures are incompetent and there is a major degree of anterior instability.
It is easy to see how one can extrapolate from this to test the anteroinferior structures, that is, by the same maneuvers in 80 degrees of abduction and stressing the shoulder down and forward compared to the opposite side. To test posterior instability, posteriorly directed translocation force is applied in different degrees of internal rotation and abduction once again comparing this to the opposite side. A chart of the results of these maneuvers on left and right sides clarifies the direction and degree of instability.
Comment
Just as it is good practice always to examine the knee under anesthesia before arthroscopy, it is always good practice to do the same -with the shoulder whether instability is suspected or not. The opportunity to examine the shoulder under anesthesia should not be missed, as often instability may be part of the problem when the patient presents with a painful shoulder. Presenting symptoms may be those of impingement, but the causation is instability. The following is an example of charting an anteroinferior instability of the left shoulder.4
External Rotation | Degrees of Rotation | Right | Left |
Anterior | 0 | 3 | 3 |
(30-Degree abduction) | Maximum | 1 | 1 |
Anteroinferior | 0 | 3 | 3 |
(90-Degree abduction) | Maximum | 1 | 3 |
Internal Rotation |
|
|
|
Posterior | 0 | 3 | 3 |
30-Degree abduction | Maximum | 1 | 1 |
Posteroinferior | 0 | 4 | 4 |
(90-Degree abduction) | Maximum | 1 | 1 |
In this example, the patient is generally quite lax and on testing in neutral has quite a marked degree of posteroinferior laxity, which is not uncommon. However, the difference between the two sides is in anteroinferior testing and shows that the left side has a degree of anteroinferior ligamentous incompetence.
Inferior Capsular Shift Stabilization
Indications
Inferior capsular shift stabilization is indicated for multidirectional instability. This has been discussed in the previous chapter and is indicated for the AMBRI end of the spectrum of shoulder instability. This type of shoulder, although loose in several directions, usually has a predominant direction of instability, which must be determined before surgery. Usually, there is a degree of congenital ligamentous laxity with an acquired repetitive microtrauma stretching of the capsule during repeated activity (e.g., backstroke swimming, bowling, and throwing sports). These patients may never have frankly dislocated the shoulder but have symptoms of recurrent subluxation or pain secondary to instability. The majority of these patients are helped by rest from the initiating cause, using a night sling to hold the arm in adduction and internal rotation to rest the capsule, and an intensive muscle-strengthening program to restabilize the joint. If all this fails after 6 months of intensive endeavor, then inferior capsular shift stabilization may be contemplated.
Preoperative Investigation
The diagnosis of multidirectional instability is made usually from the clinical history and examination. Range of motion is greater than usual. The joint can be easily passively subluxed both anteriorly, posteriorly, and inferiorly. When the joint is stressed inferiorly by pulling on the straight arm directly downward, a dip appears at the outer end of the acromion. This is the so-called sulcus sign. The position of maximal apprehension aids in the diagnosis of direction of maximal instability. On examination, these patients are often found to translocate posteriorly more than anteriorly, and yet maximal apprehension is anteroiriferiorly. Almost invariably, the approach is anteroinferior rather than posteroinferior. EUA is very helpful when compared to the other side, and arthroscopy may give confirmatory evidence by localized glenoid scuffing and chondromalacia of the humeral head rather than a Hill-Sachs deformity, which is rarely present in such cases. Anteroinferior instability is often associated with the posterosuperior synovitis. Arthroscopy also reveals a large joint volume, and the scope can be easily maneuvered from the anterior compartment to the inferior compartment without having to withdraw posteriorly. Examination while the arthroscope is in situ and stressing the joint can demonstrate anterior, inferior, and posterior subluxation.
Position of Patient
The standard beach chair position is used.
Technique
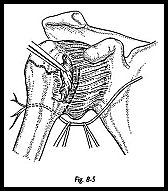
The approach down to the capsule is exactly as described in the previous section for the anterior cruciate-type repair, that is, anteroinferior deltopectoral approach, cephalic vein preserving, coracoid muscle preserving, and subscapularis divided separate from the capsule (Fig. 8-5).
On this occasion, however, the entire subscapularis is divided, and the entire inferior capsular fold must be exposed by soft tissue dissection. The axillary nerve may be palpated but must be guarded by retracting it inferiorly (Fig. 8-6).
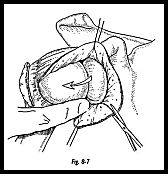
The nerve is put in a relaxed position by putting the humerus in adduction and external rotation. With a periosteal elevator, soft tissue is swept off the capsule right round the inferior surface of the neck of the humerus so that the posterior capsule itself is exposed from an inferior direction. The capsule is not opened initially in a T-shaped manner, but a vertical limb of the capsulotomy is made first (Fig. 8-7). This incision must go right up to the rotator interval superiorly and inferiorly as far as the capsule can be exposed, that is, past the 6 o'clock position on the humeral head to at least 8 o'clock posteriorly.
A stay stitch may be put in the capsule anteriorly to help provide countertraction to divide the capsule so far posteriorly. Two stay sutures are now placed in the capsule just below the meridian of the humeral head. This transverse incision is made in the capsule toward the glenoid up to the labrum.

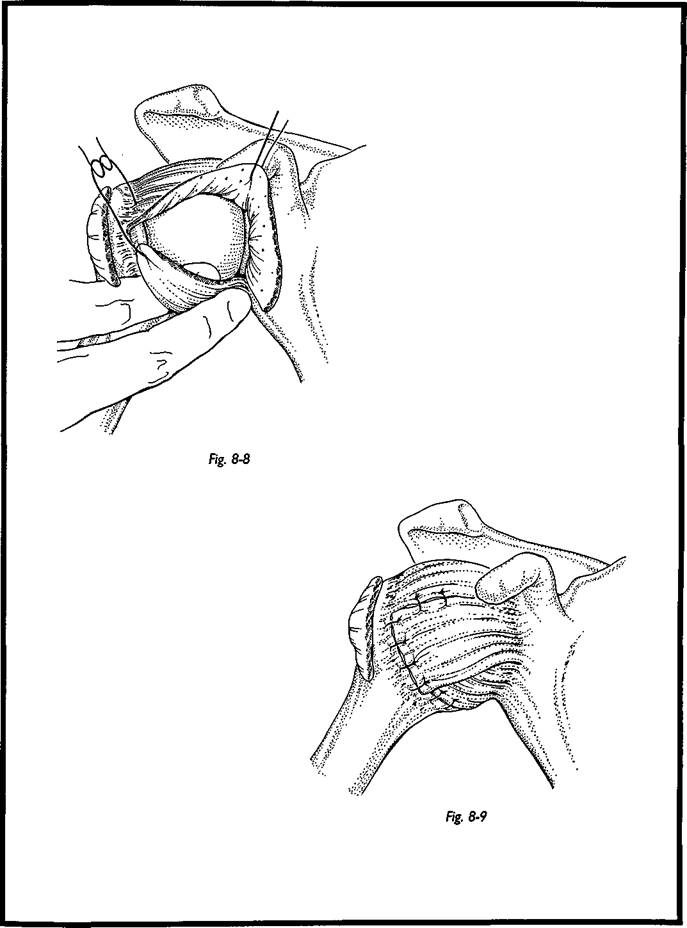
The very large inferior capsule recess may now be palpated with the forefinger and by traction on the inferior capsular stay suture it can be tested that this capsule recess can be abolished by sweeping the inferior capsule superiorly (Fig. 8-8). Often, the remaining ridge of capsule can be palpated such that the pouch remains even when applying traction to the inferior capsule. Only after this ridge is divided can the pouch be obliterated by traction on the inferior capsule.
The humeral head and glenoid are then inspected to determine that no other intra-artic-ular damage has been overlooked. Then the capsular stabilization is performed (Fig. 8-9). The inferior capsule is swept superiorly such that the apex of the inferior capsule is sutured to the posterior border of the rotator interval (the gap between the superior border of sub-. scapularis and the anterior border of supraspinatus), and the rotator interval is then closed. Additional sutures are used to fix the inferior capsule laterally and further tighten the capsule to obliterate the inferior capsule recess. When the inferior capsule has been adequately fixed, the superior capsule is swept over the inferior flap and sutured inferiorly. This gives a cruciate-type repair -with two layers of capsule anteroinferiorly.
The success of this operation depends on the spirally arranged fibers within the shoulder capsule: By pulling on the inferior capsule flap, the whole of the joint volume is diminished, such that the posterior and anterior capsule is tightened by this one maneuver, and hence even posteroinferior instability may be stabilized by this maneuver. Subscapularis is then repaired but not overlapped; it is just put back as an end-to-end repair. The deltopectoral interval is allowed to fall back into place, and the wound is closed subcutaneously and with a subcuticular suture. No drain is required.
Postoperative Management
This operation was initially described such that the patients wore a cast with the arm in slight abduction and external rotation for 6 weeks, and this is certainly necessary in the grossly congenital hyperlax patient. However, if there is no evidence of gross hyperlax-ity, a brace/sling can be used with the arm in neutral at the side, but it must be worn assiduously for 6 weeks before motion is begun. These patients never have any difficulty regaining motion, and hence early physiotherapy is related initially to restrengthening and eventually a range of motion exercises after 8 weeks.
Complications
The major complication from this procedure is damage to the axillary nerve, which is in jeopardy as it winds its way round the inferior capsule. This must be protected at all times when incising the inferior capsule. Because the operation is indicated in multidirectional instability, one must be careful to tighten the whole capsule and not just in one direction. If the anterior structures are left too tight, then posterior subluxation will result. Immediately after the capsule repair, the joint should be tested and stressed anteriorly, inferiorly, and posteriorly.
Anteroinferior Stabilization of Shoulder (Cruciate-Type Repair)
Surgical repair must be directed at the pathology that has been determined either clinically, radiographically, arthroscopically, or by surgical findings. If the anterior structures have obviously separated from the anterior labrum, they must be reattached to the decorticated anterior glenoid. However, if the problem lies mainly with the anterior capsule and glenohumeral ligaments, these must be reinforced by capsular shift-type repair. The standard utility operation for an anteroinferior instability with or without labral detachment is the reinforced capsular cruciate repair. The utility-type approach described in this section addresses each of the three following elements: (1) the Bankart lesion, (2) the capsular laxity, (3) shortening or not of subscapularis.
Indications
Anteroinferior stabilization of the shoulder is indicated for recurrent anteroinferior dislocation.
Preoperative Investigation
As previously described, immediate preoperative EUA and arthroscopy are performed.
Position of Patient
The standard beach chair position is used.
Technique
The incision is kept as far inferiorly as possible in the apex of the axilla; with the arm in full internal rotation and adduction, the apex of the axillary skin crease is marked. A line is then taken from the coracoid to this mark and then continued inferiorly. The actual incision is from the mark at the apex of the skin crease and continued 6 cm distally. Skin and subcutaneous edges are undermined by blunt dissection to reveal the deltopectoral interval, which is marked by a fatty streak and the cephalic vein.
The deltoid and pectoralis are separated by blunt dissection, preserving the cephalic vein laterally. One or two tributaries may need to be divided. A coracoid lever retractor (Copeland) is then used to retract the upper part of the wound using the coracoid as a fulcrum. The skin in the axilla is very mobile and allows this rotation very easily. A self-retaining retractor is then placed in the deltopectoral interval, and the coracoid muscles are exposed. A stay stitch is placed on the coracoid muscle, and the lateral third of the conjoint insertion is divided. This release allows adequate exposure of the more medial structures. By leaving the majority of the muscles attached to the coracoid, damage to the musculocutaneous nerve is prevented. Sometimes the musculocutaneous nerve may have a high branch into this muscle mass and may be put under considerable traction if either the coracoid or the whole muscle mass is divided and taken distally in the 'wound. The main wound self-retaining retractor is now placed such that the medial arm is deep to the coracoid muscles, exposing the subscapularis. The arm is now externally rotated, which brings the subscapularis into full prominence in the face of the wound. The superior edge of subscapularis (the rotator interval) is palpated, and the inferior margin—as demonstrated by the inferior circumflex humeral vein—shows the whole width of subscapularis.
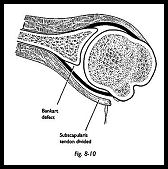
Stay sutures are then placed into the body of the subscapularis muscle itself just medial to the musculocutaneous junction. (Fig. 8-10). The subscapularis is divided separate from the capsule. While the fibers are being divided, the muscle is put under maximum stretch by putting the arm into maximal external rotation. Then as the fibers are cut, they retract and separate themselves from the underlying capsule. The muscle is divided just lateral to the musculocutaneous junction as seen by the naked eye, but as soon as the insertion is incised, then it is seen that there are muscle fibers deep to the superficial tendon. Muscle is then swept medially by blunt dissection using a periosteal elevator over a swab to push the muscle as far medially as the glenoid rim. A few fibers of the inferior part of the subscapularis are preserved along with the inferior circumflex humeral vessels. At the end of the procedure, this provides some estimate of the tension of the subscapularis and also acts as a protective mechanism for the axillary nerve.
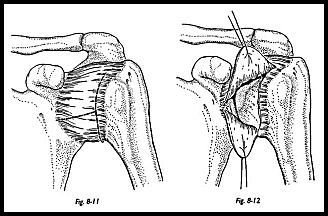
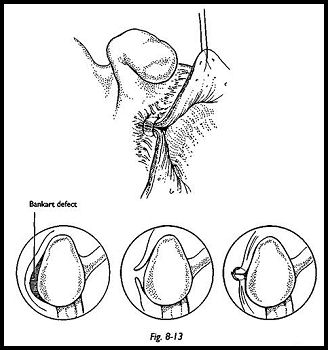
The inferior capsule recess is exposed by passing a bone lever close to the inferior capsule, again so that the axillary nerve is protected. Two short stay sutures are placed in the lateral capsule to mark the apex of the superior and inferior flaps of the laterally based T incision (Fig. 8-11). The horizontal component of the T incision is now directed to the anterior glenoid neck and deliberately into the Bankart lesion if previously identified by arthroscopy or clinical examination (Fig. 8-12).
The glenoid is then exposed using a Bankart skid to sublux the humeral head posteriorly. The glenoid neck is exposed using a spiked Rowe glenoid neck retractor driven home "with a mallet. The Bankart defect, if present, is now exposed, and the neck is decorticated using a mallet and ferret gouge or dental burr (Fig. 8-13). The three elements of stability can now be addressed.
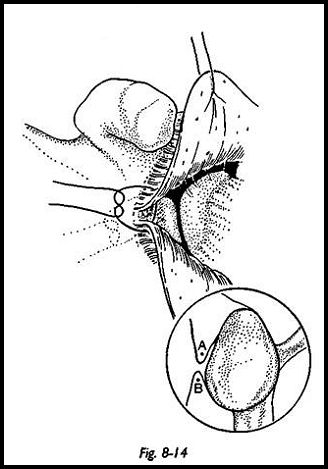
Bankart Lesion Classically, a Bankart lesion is repaired by drilling two or three holes into the articular surface of the glenoid and out through the glenoid neck. However, integrity of articular cartilage should be preserved at all costs, and the purpose is to appose the remaining labrum or capsule back to the decorticated area. This can be achieved in a number of ways without violating the articular surface. Various types of suture anchors are available commercially, but I prefer to use a vertical apical capsular suture as shown in Figure 8-1-4. The principle of which is, if the glenoid is considered a convex surface and the anterior structures are tightened, then by definition, they must come to he in apposition to the decorticated area. The suture is passed from the outside of the superior flap to the inside. If any labrum is still present, then the suture is then passed through this and then out through the inferior flap. If there is no soft tissue structure on the anterior lip of the glenoid, then the suture is just passed from outside in on the superior flap and inside out on the inferior flap, and then the suture is tied. As the suture is tied, the whole anterior capsule is seen to snug down firmly into the decorticated anterior glenoid neck. If this is not adequately firm, a further suture may be used.
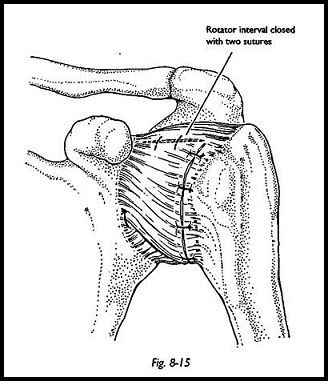
Capsular Deficiency Depending on the degree of capsular laxity, the anterior capsule is now overlapped such that the inferior capsule is taken superiorly and the superior capsule inferiorly. The inferior capsule is always much stronger than the superior, and hence the placement of the inferior capsule suture is more important. At this stage, the rotator interval is closed by taking a suture from the superior edge of the inferior capsular flap and suturing it to the posterior edge of the rotator interval (Fig. 8-15). This whole repair is done -while the arm is in some degree of abduction and external rotation. During the operative procedure, the surgeon stands in the patient's axilla such that easy control of the arm is achieved by the surgeon working with one assistant. If the surgeon always works in this position, then overtightening of the capsule and excessive internal rotation are unlikely, but at each stage of the repair, this must be checked passively. Following the completion of the capsular and Bankart repair, the shoulder should now be stable and can be tested by attempting anteroinferior subluxation with the arm in abduction and thumb pressure attempting an anteroinferior translocation.
Repair of the Subscapularis The decision needs to be taken at this stage whether to repair the subscapularis at anatomic length or to overlap it. If a large Hill-Sachs lesion (hatchet deformity) has been noted, then it is wise to deliberately limit external rotation by shortening the subscapularis. If the bony hatchet deformity in the head is not a problem, then the subscapularis does not need to be shortened and may be resutured anatomically. The coracoid muscles are then repaired, no sutures are needed for the deltopec-toral interval, and subcutaneous and subcuticular skin sutures are used.
Postoperative Management
The patient is kept in a sling with a body belt for 3 weeks with only free elbow movement permitted and no external rotation. At 3 weeks, the body belt is removed, a free sling is applied, and pendulum movement only is encouraged. At 6 weeks, a full active strengthening and stretching program is instituted, and contact sports are avoided for 6 months.
Complications
Stabilization of the shoulder is always a matter of judgment as to how much of the three elements contributes to the stability, and hence judgment depends on experience. One could obtain almost universally successful results if one s only criterion was pure stability. An arthrodesed shoulder is a totally stable shoulder, but mobility has been sacrificed. Hence, when stabilizing the shoulder, the judgment must almost always he in how to gain maximum stability while maintaining maximum mobility. An industrial worker who has had a traumatic dislocation may be quite willing to sacrifice a fair degree of mobility to ensure stability. However, a top-grade throwing athlete would be totally unable to compete again if robbed of any mobility. Hence, even in the presence of the same pathology, the operative procedure must be tailored to the needs of the patient. Complications occur when this judgment is wrong. Hence, the patient will be dissatisfied if there is any unnecessary loss of motion, particularly external rotation. It has been shown that a long-term incidence of osteoarthritic change can be directly related to the degree of loss of external rotation. Recurrent dislocation that may occur in the overall incidence is approximately 5 percent. If these patients return to contact sports, they will be in danger of redislocating the shoulder again if the same accident recurs.
Modified Bristow-Helfet Anterior Stabilization
The Bristow procedure involves the transfer of the distal portion of the coracoid process with the attached conjoined tendon to the anterior aspect of the scapula neck through a transverse opening in the subscapularis muscle. The procedure was described by Helfet and is commonly known as the Bristow procedure,5 but in fact, a similar procedure was described by Latar jet four years earlier in 1954 and hence is also known as the Latarjet procedure.6 The operation is thought to work in several different ways: (1) as an anterior bone block; (2) in abduction external rotation, that is, the position of instability, the restraining bow string keeps the head from sublux-ing anteriorly; (3) the subscapularis is prevented from rolling superiorly, and the lower third of the subscapularis is pinned down as a tenodesis.
Indications
The Bristow-Helfet procedure is very useful for the recurrent anterior instability of the traumatic type that previous surgery has failed to correct and scarring is such that a more sophisticated procedure is difficult to perform. In the presence of any element of anterior glenoid insufficiency, the bone block effect of this procedure can be useful.
Contraindications
The Bristow-Helfet procedure should not be used in throwing athletes because they cannot return to preinjury status. Anatomy is altered, and there is relative shortening of subscapularis muscle and therefore loss of internal rotation power. If this procedure fails, then reconstruction can be difficult because of the altered anatomy and intense scarring that this procedure can produce. This operation is not indicated for multidirectional instability or in patients whose anterior instability is reproduced with the arm at the side.
Preoperative Investigation
Routine examination under anaesthesia before stabilization and arthroscopy can confirm the intra-articular pathology and in particular the state of the anterior glenoid.
Position of Patient
The standard beach chair position is used with a sand bag under the medial border of the scapula to thrust the shoulder forward.
Technique
An anteroinferior approach is used as in the previous two sections.
The deltopectoral interval is found and separated by blunt dissection, preserving the cephalic vein. The coracoid process is then identified, the coracoid lever retractor (Copeland) is inserted to retract the superior wound edge, and the conjoined tendon is identified. The conjoined tendon should be isolated medially and laterally. Usually, a small strand of muscle lateral to the short head of biceps marks the lateral extent of the conjoined tendon. This step is necessary to allow the distal reflection of the coracoid process and conjoined tendon as one unit to permit adequate visualization of the underlying subscapularis muscle. The fascia overlying the superior aspect of the coracoid process is reflected 1 to 1.5 cm from its tip. This helps to delineate the area of the coracoid process that will be osteotomized and reflected with the attached conjoined tendon.
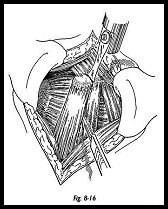
It is easier to drill the coracoid at this stage before osteotomy. An AO malleolar screw is used for fixation (Fig. 8-16). The coracoid process is osteotomized 1 cm at proximal to the tip. The coracoid is palpated, and the osteotomy is made with a power saw at right angles to the coracoid itself to avoid leaving an oblique surface. If a small spike of bone remains on the coracoid process, it should be removed with the use of a rongeur to leave a completely flat and smooth surface to permit proper contact with the anterior surface of the glenoid neck when the transfer is complete.
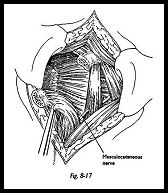
The coracoid process and conjoined tendon are reflected distally to permit visualization of the underlying subscapularis and subscapularis tendon and muscle. Distal traction should not be applied to the coracoid, because this can inadvertently place traction on the musculocutaneous nerve, which can enter the conjoined tendon 2 to 8 cm distal to the coracoid process (Fig. 8-17). Once the coracoid process and tendon are reflected distally, they should be placed within the depth of the wound.
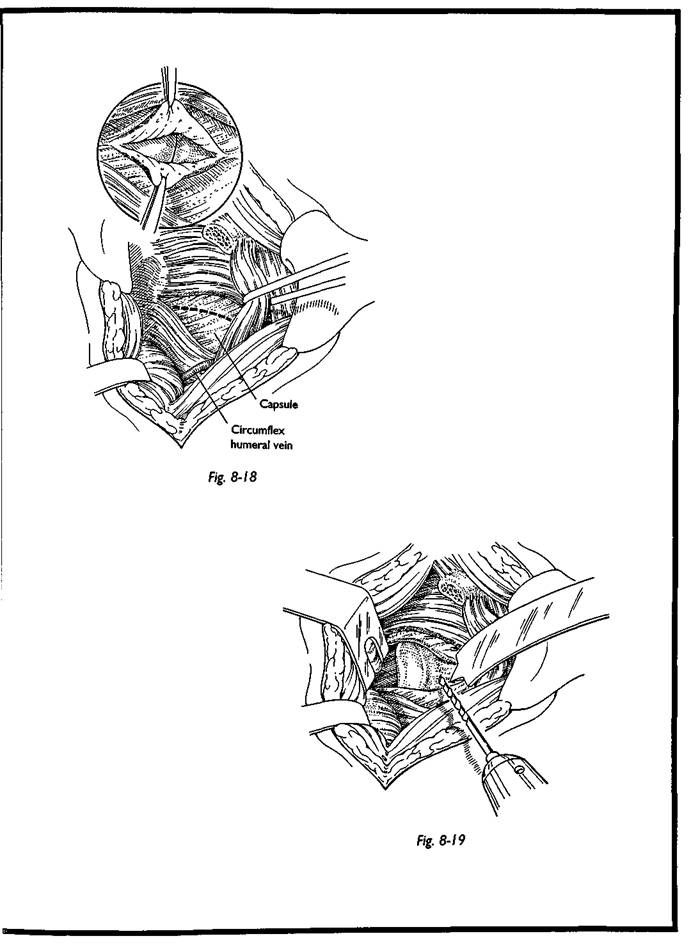
The upper and lower limits of the subscapularis muscle are identified by palpation. The lower border of the subscapularis is identified by the circumflex humeral veins. The upper border of subscapularis is easily identified at the rotator interval. The subscapularis muscle is split in line with its fibers from lateral to medial at the junction of the middle to lower third of the muscle. While doing this maneuver, the surgeon should palpate the anterior lip of the glenoid. To do this, the arm needs to be repeatedly internally rotated because external rotation can induce some degree of anterior subluxation of the humeral head, making the glenoid rim difficult to palpate.
The joint is then entered by sharp dissection onto the anterior face of the glenoid neck, where a Bankart lesion may well be present (Fig. 8-18). The labrum and capsule on the anterior surface of the glenoid and scapula neck are incised and reflected superiorly and inferiorly. The glenoid neck is now exposed using a Rowe pronged retractor or devil's pitchfork; this step must be done under direct vision. A 3.2-mm hole is drilled in the anterior-to-posterior direction of the glenoid neck, parallel but 1 cm medial to the articular surface (Fig. 8-19). Good visualization of the articular surface of the glenoid is achieved by posterior subluxation of the humeral head with a Bankart retractor. The drill must pass through both cortices of the glenoid neck and depth gauge used to measure the length of the hole. This measurement is then added to the depth of the coracoid fragment, and the appropriate length screw is selected.
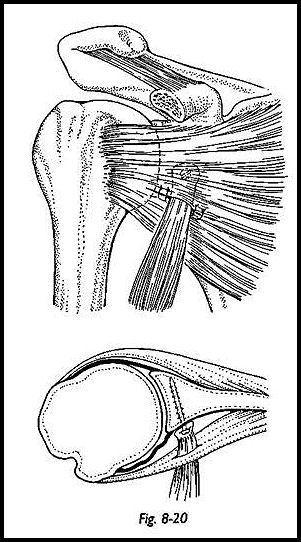
Care must be taken not to allow the screw to protrude posteriorly, and hence the screw size below the combined lengths is used. Any posterior protrusion of the screw can cause posterior scapula discomfort. The screw is passed through the coracoid fragment such that the fragment is on the smooth part of the shank of the screw. The threaded part of the screw is then aimed into the hole in the glenoid neck, and the coracoid fragment is screwed down so that there is cancellous apposition between the Bankart defect and the bony fragment (Fig. 8-20). Once the screw is in place and the bone block fixed, the surgeon should check that there is no overhang of bone over the glenoid rim. If there is, then the screw should be loosened and the bone block rotated so that the narrowest portion of the bone block lies lateral to the screw. The fascia overlying subscapularis muscle should be reapproximated with two absorbable sutures, and the 'wound then should be closed in layers (Fig. 8-21).
Postoperative Management
A sling is used for 3 'weeks with a body belt; elbow and hand motions are begun on the first day; pendulum exercises at 3 weeks; and formal range of motion and strengthening exercises only started at 6 weeks. Noncontact sports are permitted at 3 to 4 months, but contact sports at 6 months. A postoperative radiograph should be taken to ensure proper placement of bone block and screw before the patient is allowed to return to full activities.
Complications
The most common complication described is migration of the bone block and/or migration of the screw. If at the time of surgery the bone block is split when tightening the screw, some other form of fixation must be used, that is, staple or suture fixation alone. Damage to the musculocutaneous nerve by overvigorous distal traction on the separated coracoid is a complication but usually only causes a transient palsy. Proper placement of the bone block and screw is in the middle-to-lower equatorial position of the anterior surface of the scapula neck and within 5 mm of the articular surface of the glenoid. One of the largest series reported is that by Hovelieus et al. in 1983 with a redislocation rate of 6 percent in 112 cases after a 30-month follow-up.7 The best results were in those patients in whom the bone block was placed on the inferior half of the glenoid rim within 1 cm of the glenoid surface.
References
1. Neer CA, Fithian TE, Hansen PE et al. Re-inforced capsular cruciate repair for recurrent anterior dislocation of shoulder. Orthop Trans 9:44, 1984
2. Turkel SJ, Panio MW, Marshall JL, Girgis FG: Stabilising mechanism preventing anterior dislocation of the gleno-humeral joint. J Bone Joint Surg [Am] 63:1208—17, 1981
3. O'Brien SJ, Neves MS, Rozback RS et al: The anatomy and histology of the inferior gleno-humeral ligament complex of the shoulder. Paper presented at the Annual meeting of the Shoulder and Elbow Society, February 1989, Las Vegas.
4. Cofield RH, Nessler JP, Weinstabl R: Diagnosis of shoulder instability by examination under anaesthesia. Clin Orthop Rel Res 291:45-53, 1993
5. Helfet AJ: Coracoid transplantation for recurring dislocation of the shoulder. J Bone Joint Surg [Br] 40:198-202, 1958
6. Hovehus L et al: The Bristow-Latarjet procedure for recurrent dislocation of the shoulder. A two-five year follow up study on the results of 112 cases. Acta Orthop Scand 54:284-90, 1983
Suggested Reading
Ribbans WJ, Mitchell R, Taylor GJ. Computerised arthrotomography of primary anterior dislocation of shoulder. J Bone Joint Surg [Br] 72:181-6, 1990


