Rotator Cuff Repair
Acute tearing of the rotator cuff is a rarity in a younger person with good muscle. The more common injury in the young is avulsion of one of the tuberosities because the tendon is stronger than bone at this site. Occasionally, however, a true acute tear occurs, and in a younger person, this must be diagnosed early and repaired as soon as possible.
The opposite end of the spectrum of disease is the very elderly patient in whom the rotator cuff may almost dissolve away with attrition rupture almost painlessly. Rotator cuff ruptures are noted in autopsy studies of cadavers with an incidence ranging from 24 to 80 percent. Hence, not all rotator cuff ruptures are painful, and it is not known what makes some rotator cuff tears painful and some not. The majority of tears he somewhere in the middle of this spectrum of disease, but usually an element of trauma is superimposed on an already chronic degenerative musculotendinous junction.
The relative merits of the causative factors of this degenerative change are debatable and include primary collagen degeneration, vascular attrition, and mechanical factors (i.e., hooked acromion), but the final common pathway appears to be mechanical impingement under the anteroinferior acromion as described by Neer. Hence, decompression of the rotator cuff must be part of any rotator cuff repair. There is little point in repairing the cuff and then returning it to its same physiologic environment, which had brought about progressive weakening of the musculotendinous junction. The disease process must be halted and indeed reversed if possible. Impingement must be abolished by an anterior acromionectomy and excision of the coracoacromial ligament. All effort must be made to bring in a new blood supply to the ruptured area, usually by putting the repaired edges of the muscle down to a bleeding cancellous area of bone and making every effort to preserve the vascular subacromial bursa, so that this may bring in a new blood supply. The bursa may be likened to the omentum in the abdomen, which has been called the policeman of the abdomen because of its ability to stop trouble at an early stage by providing a mobile and new blood supply. Microscopically, the subacromial bursa is an extremely vascular structure, and this property may be used in the repair.
The primary goal of surgery is to relieve the patient's pain and secondarily to improve function, strength, and range of movement. The two factors of injury and degenerative change must be assessed, and hence in treatment of the younger patient, the tendency is toward earlier surgery. In the older patient, less radical surgery should be contemplated if possible. Initially, in older patients, a nonopera-tive program is started with a trial of physiotherapy, stretching, and strengthening; nonsteroidal anti-inflammatory agents may be used; and even injections may prove beneficial. Night pain is a common feature of a rotator cuff tear; this usually reflects the inflammatory element of the problem. Although a local steroid in the presence of a disrupted tendon may in theory be ill-advised, it is often extremely beneficial in the very elderly and may be adequate to sufficiently relieve their symptoms for non-operative treatment, but no more than three injections should be contemplated (see Ch. 2).
Indications
As suggested above, rotator cuff repair is indicated for acute and chronic rotator cuff tears. The postoperative regimen must be discussed -with patients in detail, so that they understand how this will affect their activities of daily living over several months. Patients must be fit and well enough to comply with a protracted physiotherapy regimen. In the very elderly in whom pain is the main feature and 'who are not concerned about loss of range of movements or power, it may be wiser to consider decompression and debridement only. This may be done by open surgery or arthroscopically and has a reasonable success rate. If this were to fail, then formal cuff repair may have to be considered.
Contraindications
Repair in the very elderly and infirm is not wise if they are unable to follow the extensive postoperative program. In the elderly, if the shoulder is painless but has poor range of movement and strength, then it is unlikely that repair of the cuff will provide them ¦with sufficient increase of range of movement and strength. Surgery may even make a previously painless shoulder painful.
Preoperative Investigation
The diagnosis is predominantly clinical, that is, a history of night pain, a previous history of shoulder disability with superimposed injury, and sudden loss of power of external rotation and elevation. It must be stressed that patients present with a wide range of symptomatology, and a high index of suspicion must be maintained in face of sudden onset of pain in the elderly. It is perfectly possible to have a full range of movement in the presence of a full-thickness rotator cuff tear. The most sensitive index is loss of power of external rotation in approximately 30 degrees of abduction when compared with the opposite normal side. If the cuff tear is large and the patient of a thin aesthenic build, then the tear itself may be easily palpable by feeling just lateral to the acromion and rotating the arm underneath the palpating finger.
Plain Radiography
Plain radiography is often extremely helpful and may show signs of obvious rotator cuff tear, i.e. elevation of the humeral head such that the humerus is abutting on the under surface of the acromion, but by the time this is happening the clinical diagnosis should be obvious. More subtle changes of the rotator cuff in distress are sclerosis on the under surface of the acromion and the greater tuberosity, cystic change in the greater tuberosity, anterior acromion spurring and osteophyte changes on the under surface of the acromioclavicular joint.
Arthrography
Arthrography is the most definitive investigation to determine whether a full-thickness tear is present. If dye injected into the glenohumeral joint enters the subacromial bursa, then by definition there must be a rotator cuff tear. If the question is only Is there a cuff tear or not? then arthrography is the most reliable investigation. If a double-contrast arthrogram is combined with tomography, then some assessment can be made as to the size and position of the tear.
Ultrasound
Ultrasound is widely used and in the best hands almost as accurate as arthrograpy in diagnosing a full-thickness rotator cuff tear. Ultrasound, however, is not accurate in assessing a partial thickness tear and is extremely operator dependent, yielding reasonable results in skilled hands and most unreliable results with the less experienced. Ultrasound is a good, cheap, readily available, noninvasive alternative.
Magnetic Resonance Imaging
Alagnetic resonance imaging is an excellent method of assessing the rotator cuff but does need experienced interpretation. Size and site of cuff tearing can be accurately estimated, and this is the only investigation that can give a good assessment of partial thickness tearing and intrasubstance tears.
Arthroscopy
Sometimes a rotator cuff tear may be found on arthroscopy when not clinically suspected. Arthroscopy is an excellent way of assessing partial bursal thickness and articular surface tears.
Position of Patient
The standard beach chair position is used (see Ch. 1, Fig. 1-8).
Technique
The superior strap incision is used with the superior deltoid splitting approach (see Ch. 1. Figs. 1-20 to 1-22). The strap approach is useful for rotator cuff repairs, because this can be extended when the extent of the tear has been fully recognized. Initially, exactly the same approach is used as for an open decompression procedure: that is, the superior strap incision and a small anterior deltoid split incision with minimal detachment from the anterior acromion.
The acromioplasty is then done, removing the anteroinferior third of the acromion 'with the coracoacromial ligament (see section on decompression acromioplasty). The inferior surface of the acromioclavicular joint is palpated, and if an inferior osteophyte is present, this too is trimmed. If at clinical examination, an injection had indicated acromioclavicular joint problems, then an acromioclavicular excision arthroplasty removing the outer centimeter of the clavicle may be accomplished at this stage but is not necessary as part of the exposure of the cuff. The subacromial bursa is incised, but preserved as much as possible. Part of the bursa is inevitably removed because it is closely apposed to the undersurface of the coracoacromial ligament. The bursa is an extremely elastic structure, and every effort should be made to close this at the end of the procedure. The small initial mini-split approach is used to assess the size of the tear by rotating the arm underneath the window through the split in the deltoid. If the tear is small, then it can be repaired through this minisplit. If it is a large tear, then the strap incision may be extended either anteriorly or posteriorly and deltoid split to 5 cm from the anterior edge of the acromion. A suture may be placed around the deltoid at the distal end of the split to prevent propagation of the split and causing possible damage to the axillary nerve.
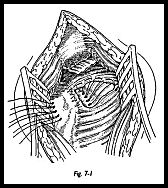
Superoposteriorly, the wound may be extended such that deltoid is taken off from the acromion with an osteoperiosteal flap laterally, and the flap is raised on the acromion also with an osteotome to allow closure at the end of the procedure (Fig. 7-1). Only the minimal amount of the deltoid is detached from the acromion to allow for the rotator cuff closure.
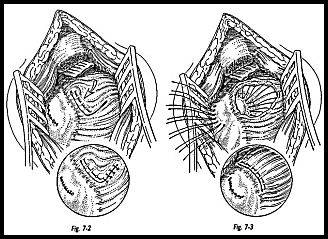
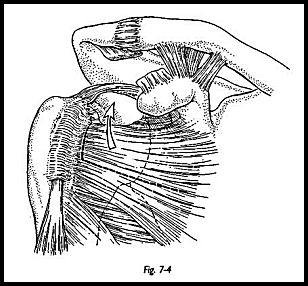
A large cuff repair can be repaired through minimal exposure with adequate positioning of the arm (Fig. 7-2). A small traumatic avulsion tear can easily be directly repaired, either side to side or end to end (Fig. 7-3). For the moderate-size tear, mobilization of the cuff may be required to facilitate closure. Sometimes the tear will appear to be so massive that it is thought to be impossible to close. However, with experience, the majority can be closed with patience and adequate mobilization of the scarred degenerate cuff. Multiple stay sutures are placed in any edge of rotator cuff that is seen, and then sequential traction is applied so that the apex of the tear may be identified. Care must be taken to ensure that the sutures are put in rotator cuff and not in thickened fibrosed subacromial bursa. Sometimes the cuff can be so atrophic that differentiation anteriorly may be difficult.
Local Muscle Flap Repair
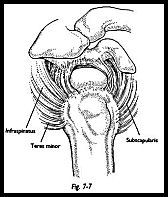
Tear of the rotator cuff complex almost invariably includes the supraspinatus tendon, but the tear may include other tendons also. It may extend posteriorly to involve supraspinatus or anteriorly to involve subscapularis. Rarely, it may be a complete "bald head" tear extending in both directions. Ideally, the rotator cuff defect should be closed by direct repair alone. Anything less than this means accepting some degree of functional loss. If the defect cannot be closed by direct repair alone, then the simplest method is to use a local muscle flap. Most commonly, this is subscapularis swung superiorly and posteriorly; less often, infraspinatus can be used.
Indications Local muscle flap repair is indicated for moderate-to-large rotator cuff tears (see Ch. 7).
Position of Patient The standard beach chair position is used.
Technique The superior strap approach is used (see p. 72). The rotator cuff is exposed, and the size of the defect is assessed. The edges of the defect are tagged with stay sutures, and the entire rotator cuff is mobilized as much as possible posteriorly, medially, and anteriorly. The retracted tendon is incised free from the base of the coracoid to allow mobilization laterally from the retracted position. Once maximum mobilization has been obtained, then trial closure using tension on the stay sutures is attempted.
The superior strap approach is used (see p. 72). The rotator cuff is exposed, and the size of the defect is assessed. The edges of the defect are tagged with stay sutures, and the entire rotator cuff is mobilized as much as possible posteriorly, medially, and anteriorly. The retracted tendon is incised free from the base of the coracoid to allow mobilization laterally from the retracted position. Once maximum mobilization has been obtained, then trial closure using tension on the stay sutures is attempted.If tension applied to the posterior cuff can be brought to the midline superior position but still leaves a defect anteriorly, then a subscapularis muscle flap transfer may be the option of choice (Fig. 7-4). The superior half to two-thirds of subscapularis may be transferred superiorly. The intention is to transfer the muscle, but to leave the capsule intact to keep the shoulder stable. The line of incision of subscapularis muscle extends from superolaterally to inferomedially separating muscle from tendon (Fig. 7-5).
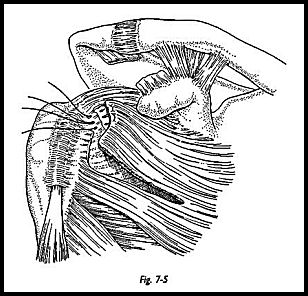
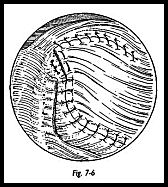
Traction sutures are then placed in the free edge of the subscapularis tendon and the transposed tissue positioned and sutured in place. The medial aspect of the superior edge of the subscapularis muscle is sutured to the remaining supraspinatus and infraspinatus muscle over the superior aspect of the glenohumeral joint (Fig. 7-6). The tendon-to-bone repair is performed, and then further tendon-to-tendon sutures are placed over the superior aspect of the humeral head and along the subscapularis incision. Tendon-to-bone sutures are placed by exposing a trench of cancellous bone on the humeral head.
The location of the trench is determined by placing the arm in 20 degrees of abduction and applying tension to the traction sutures. The cancellous bone is then exposed medial to the point reached by the transposed tendon edge. The anteroposterior length of the bony trench approximates to the length of the original tendon disruption from its bony insertion. Sutures are placed through bone, through tendon, and then tied. The repair should be secure with the arm at the side and should allow for external rotation of 20 to 30 degrees.
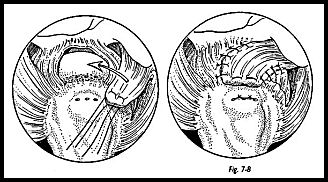
If the defect in the rotator cuff lies more posteriorly, then a similar flap of infraspinatus may be swung up superoposteriorly, although this is less often used than the subscapularis flap (Figs. 7-6 to 7-8).
Postoperative Management It is important to examine the shoulder movement after rotator cuff repair but before deltoid closure. This allows the postoperative program to be planned and the physiotherapy program individualized. After sub-scapularis tendon transfer, the repair is usually most relaxed with the arm near the side and the internal rotation. A sling with body belt is used for 6 weeks, and during this time, only passive movements are allowed. Passive assisted exercises are performed for 6 to 8 weeks, and at 8 weeks, active movements are begun. This is an average program for a moderate-to-large rotator cuff tear but can be varied as to the security of repair.
Management of Massive Irreparable Rotator Cuff Tears
When a cuff tear is first exposed, it often looks irreparable, but with experience and patiently immobilizing the tendon, the vast majority of cuff tears can be closed by either direct suture or local muscle flap transfer. However, occasionally, particularly in the elderly, a gross bald head tear must be deemed irreparable. In this situation, it may be preferable to abandon attempts at repair and just to debride the remains of the cuff and decompress. This may give adequate pain relief alone. However, this will not restore obviously better function or range of motion. An alternative is to use a more distal muscle transfer, for example, latissimus dorsi transfer described by Gerber et al.1 Although this is big surgery, the results have certainly been encouraging.
Mobilization of the Rotator Cuff
Once multiple stay sutures are in situ, blunt dissection is used to break down adhesions of the retracted tendon. The 'whole cuff must be treated symptomatically by working around the stay sutures and putting traction sequentially posteriorly, centrally, and anteriorly. The finger is swept around superficial to the infraspinatus and deep to the deltoid posteriorly and then over the supraspinatus and subscapu-laris anteriorly.
In a large rotator cuff tear, the single most useful maneuver is to detach the retracted cuff from the base of the coracoid process. This can be done by sharp dissection and then using the periosteal elevator, sweeping down the body of the coracoid to detach the muscle off the base. This maneuver allows lateral mobilization of the whole rotator interval area. Care should be taken not to go medial to the coracoid for fear of endangering brachial plexus and axillary artery.
Attention is now paid to the undersurface of the cuff. If the cuff tear is massive, then a humeral head retractor may be placed through the cuff tear, hooked onto the inferior Kp of the glenoid, and the humeral head may be subluxed inferiorly. Infraspinatus may be released from the glenoid posteriorly and by sharp dissection swept round superiorly and anteriorly if more mobilization is required. It must be stressed that this maneuver is only required in the massive rotator cuff tear and is not routine.
Repair of the Tendon
After mobilization of the cuff as maximally as possible, tension on the stay sutures will show what can be reasonably achieved under moderate tension. The cuff may tear in a large variety of ways. A true semicircular avulsion from the tuberosity may occur, or there may occur a vertical split in the line of the fibers with an added tuberosity avulsion such that the defect is L shaped. Only by experimenting with the tension in the stay sutures can this be fully explored.
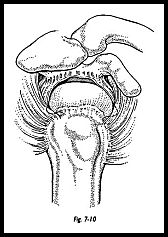
In the vast majority of patients, the repaired tendon must be put down to a bony trough in the humeral head. This bony trough is partly to provide a new blood supply from the bleeding cancellous bone and partly to release tension in the repair such that the trough is made at the site to where the muscle can be brought with reasonable tension (Fig. 7-9). If this means sacrificing superior articular cartilage, then this is a better option than either extensive muscle flaps, or nonphysiologic muscle tension. The trough is fashioned with a gentle slope toward the articular surface (Fig. 7-10). The apex of the tear is identified and repaired with number 1 monofilament PDS suture.
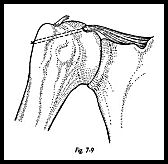
There is much debate as to the correct suture to be used in this situation. I prefer an absorbable suture, and although PDS does stretch, I feel it is an advantage to be a little forgiving in this area.
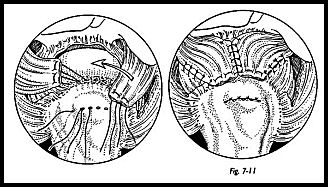
Finally, the cuff is sutured down to the bony trench with sutures passed through the bone (Fig. 7-11). The cancellous bone in the tuberosity region can be very soft, and care must be taken to try to preserve the bony bridge between the suture. A Mason Allen grasping-type suture is used in the rotator cuff itself. Various commercially available loop suture passers can aid the passing of sutures through the bone and can be very useful. A sharp trocar pointed needle, however, can be used to directly pass suture through bone in most cases, because the bone in this region is relatively soft. Suture anchors have been used in this site, but not uniformly successfully because of the poor quality of bone.
Although the repair must be adequate when finished to allow the arm to be adducted and internally rotated at the side, during the actual tying of the knots, the shoulder may be abducted and externally rotated.
Closure of the wound is an extremely important part of this procedure. First, every effort is made to repair the subacromial bursa for two reasons. (1) to provide a gliding surface between the repair and the undersurface of the acromion and (2) to provide a new blood supply to the repaired area. The deltoid is reattached to the acromion, either directly to the periosteal flap or through drill holes in the acromion. Whatever method is used, the repair must be secure to allow for early mobilizing and rehabilitation. Deltoid avulsion from the acromion is a disaster that must be avoided at all costs.
Postoperative Management
An abduction brace is not used routinely, although they are widely used. I prefer to use a sling with the arm at the side and to pursue early passive mobilization. If the repair was unavoidably under great tension, then an abduction pillow may be used, but if the decision is made to use a pillow, then it must be kept for at least 6 weeks after reconstruction. The repair is at its weakest at approximately 10 to 14 days, and this is not the time to remove the abduction pillow. Until 3 weeks have elapsed, only pendulum movements and passive flexion extension in the scapular plain are allowed. Between 3 and 6 weeks, a greater range of passive mobilizing is allowed; at 6 weeks, passive assisted exercises are started; and at 8 weeks, active exercise is allowed. This routine is modified in the hght of the security of the repair and must be individualised to each patient. Only the surgeon can prescribe the exact physiotherapy routine following surgery. Patients are told that the shoulder will continue to improve in both strength and mobility for 18 months after the repair, although the majority of gains are within the first 6 months.
Reference
1. Gerber C, Vinh TS, Hertez R: Latissimus dorsi transfer for the treatment of massive tears of the rotator cuff. Clin Orthop 232:51-61, 1988
Suggested Readings
Cofield RH: Current concepts review: rotator cuff disease of the shoulder. J Bone Joint Surg [Am] 67:974-9, 1985 Neviaser RJ, Neviaser TJ: Major ruptures of rotator cuff. In Watson M (ed): Practical Shoulder Surgery. Grune & Stratton, Orlando, FL, 1985


