Excision Arthroplasty of the Sternoclavicular Joint
Indications
Sternoclavicular Osteoarthritis
A swelling over the sternoclavicular joint is almost a normality with increasing age, but sometimes degenerative change does cause pain. The onset of swelling over the sternoclavicular joint can be quite rapid in the elderly, such that neoplasm may be suspected and biopsy carried out. Unless there is clear radiographic evidence of progressive bony destruction, then biopsy can be avoided, and the condition treated expectantly. However, if pain is the presenting symptom and is relieved by local anesthetic, excision arthroplasty of the sternoclavicular joint may be considered.
Old Traumatic Sternoclavicular Dislocation
In the majority of patients, old traumatic sternoclavicular dislocations are asymptomatic and require no treatment. However, sometimes these can lead to hypertrophic degenerative change requiring treatment. If the inner end of the clavicle is essentially stable, then excision only will be satisfactory. If it is unstable, then stabilization of the medial end of the clavicle must be considered.
Contraindications
Sometimes in the hyperlax individual, the sternoclavicular joint may be voluntarily dislocated. Usually, this is a painless procedure followed by a loud click or thud. Surgery of this condition is contraindicated because the proximal clavicle will remain unstable and will then be dislocatable voluntarily. Very rarely as a patient ages, the voluntary dislocation may be accompanied by increasing pain, at which stage the incentive to dislocate it is much less and the chances of successful surgery will increase; excision arthroplasty may then be considered.
Preoperative Investigation
Standard anteroposterior plain radiographs are difficult to interpret because of overlying rib shadows.
Anteroposterior tomograms of sternoclavicular joints are probably the most useful investigation to delineate the degree of degenerative change or subluxation.
If local anesthetic is injected into the sternoclavicular joint itself and abolishes pain, this gives a good indication that excision arthroplasty will succeed. A joint will only accept 1 or 2 ml of local anesthetic.
Procedure
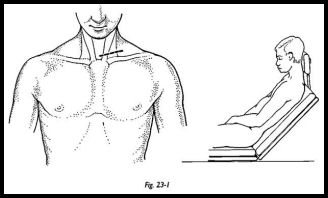
The patient is placed in the standard shoulder position with the arm draped free, but with the head cocked forward to relax the skin over the front of the neck (Fig. 23-1). An oblique incision is made in the necklace line approximately 2 cm superior to the sternoclavicular joint. This incision is chosen because transverse incisions in the base of the neck heal extremely well, whereas transverse incisions over the front of the chest heal badly and are prone to keloid scar formation. The incision is made and retracted interiorly to expose the sternoclavicular joint.
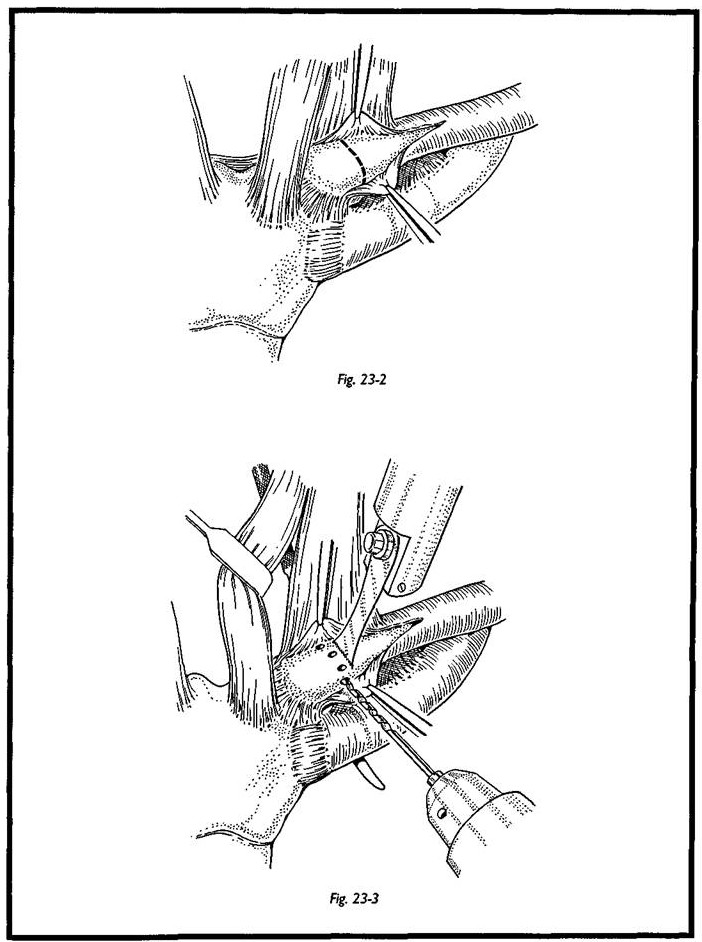
The periosteum is incised transversely, and part of the clavicular head of sternomas-toid is elevated with the periosteum. The inferior periosteum is very carefully elevated to ensure that the stabilizing costoclavicular ligaments are not damaged. When elevating the periosteum on the deep surface of the clavicle, the utmost care must be taken because the immediate deep relation to the sternoclavicular joint is the innominate vein and catastrophic hemorrhage could result (Fig. 23-2). The rougine therefore is kept on bone all the way round until eventually the medial end of clavicle is exposed. This periosteum is easy to elevate approximately 1 cm along the clavicle from the sternoclavicular joint, but there is a very deep attachment at the sternoclavicular joint itself. This may be left in situ until the clavicle is divided (Fig. 23-3).
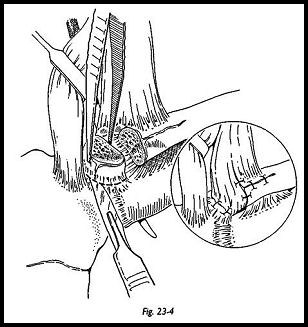
A narrow periosteal elevator or bone lever is passed behind the clavicle to protect the deep structures, and the clavicular osteotomy is made with an oscillating saw (Fig. 23-4). The proximal fragment may then be levered up and either be removed in one piece or removed piecemeal, which may be safer. The deep capsule of the joint is left in situ. An attempt is made to fill the gap with surrounding soft tissue. The elevated part of ster-nomastoid is transposed into the space and sutured between the bone ends.
The wound is closed with meticulous hemostasis and subcuticular suture after checking that the medial end of the clavicle remains stable.
Complications
Possibility of Hemorrhage
Because the relationship to the great vessels is so well-known, this is a very rare complication. One tends to be rather overcautious than overconfident in this area.
Instability During the Procedure
It is possible to divide the costoclavicular ligaments and hence destabilize the medial end of the clavicle. If this is recognized at the time, then the joint must be stabilized by repairing these ligaments with a through-and-through bony suture.
Keloid Scar Formation
Keloid scar formation can be avoided by trying to keep the scar at the base of the neck rather than over the anterior chest wall. The skin in this region is much less prone to keloid formation. Any transverse scar centered directly over the sternoclavicular joint itself is very prone to stretching and keloid.
Suggested Reading
Rockwood C: The Shoulder. WB Saunders, Philadelphia, 1990


