Post op Shoulder Rehab
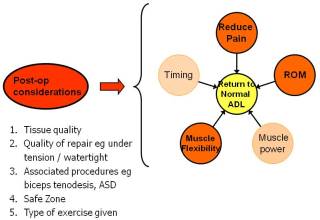
This article discusses basic principles of rehabilitation of the shoulder after surgery. These principles are the ones I use myself and apply to all of my own patients. They are interchangeable and the bias changes depending on the demand of the patient and their needs as well as the stage of recovery. There is no one aspect that is more or less important than another, but each have an impact on the progress and each can contribute to lack of progress. The key is to find which one has the greatest influence at any one time and address that in order to achieve the others.
For example, increased pain will:
- prevent muscle from working efficiently therefore limiting strengthening programs
- limit active ROM preventing functional use of arm and can affect muscle power in end ranges
- increases muscle tightness as a protective response thereby reducing flexibility
Reduced timing of muscle action can:
- increase pain within certain aspects of ROM or activity
- alter muscle flexibility in neighbouring muscle groups as they try to compensate for under or over activity in affected muscle groups.
- produce abnormal functional pattern resulting in poor feedback and so the cycle continues
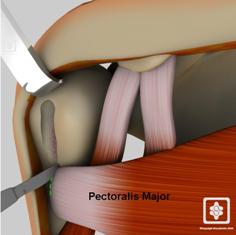
The surgical procedure and tissue involved need to be taken into consideration. It is vital to have an understanding of the surgical procedure and the limitations is will subsequently place on rehab as well give understanding of the aims of the procedure. Open procedures will inevitably involve dissection of muscle tissue/ tendon to provide access to the joint therefore when you are rehab you need to add this component into the mix as well as the specific tissue involved in the initial procedure.
Debridement / Excisional Procedures:
eg. subacromial decompression, AC joint excision, MUA, capsular release, microfracture

With these procedures the primary aim is to regain correct ROM as soon as possible. Common associated problems include movement dysfunction of shoulder complex, poor postural position, dysfunctional rotator cuff. AC joint often associated with ASD procedure patients also tend to have more problems with post op pain than the average ASD alone. There are very few limitations with these procedures other than excessive activity / strengthening with overhead movement.
Repair Procedures
eg. rotator cuff repair, stabilisation, shoulder replacement, fracture fixation.
Things to keep in mind:
- Tissue stretch does the exercise you are doing cause a stretch in repaired tissue yes? How much? Direction of stretch? Is it safe?
- Contraction is the muscle expected to actively work? Yes? How? Is it safe?
- Starting position is the muscle at an advantage? In a neutral position? At a disadvantage? See exercise booklet
- Tendon healing evidence to show tendon repair is improved if they are subjected to controlled stress in contractile and stretch directions.
Stabilisation Procedures / Labral Repairs:
With stabilisation patients there is a high association of poor core control, scapula dysrhythmia sometimes general laxity, as well as issues with the rotator cuff recruitment during active movement. These need to be taken into account and form aspects of the rehab program. Meaning that these can be addressed while the sling is in situ eg gym ball core work in sitting, lunges, single leg squats etc.
Careful consideration need to be taken when there is a combination, ie anterior and posterior repairs. You need to work in stress free ROM (safe zone) and therefore the patient is the best guide. All techniques need to be pain free and with minimal stretch, watch out for rotation in normal ROM - remember Codmans paradox.
The general ranges to avoid (beyond safe zones) are:
- Anterior repairs - combined abduction with ER
- Posterior repairs - combined flexion with IR
- SLAP repair - ER with arm in 15° abd
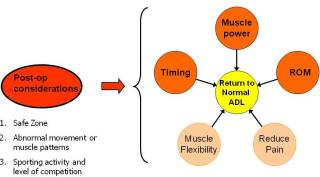
Goal Setting
General guidelines can be designed with the average person in mind and with the natural limitations of the tissue repair involved. See Shoulderdoc and GOST protocols as an example.
Goal setting should be individualised and specific. Part of the rehab should be practising activity common to the person's lifestyle. Keeping in mind full ROM required for activity, speed of movement and precision needed to perform task.
Considerations include:
- Previous level of activity
- General fitness / Physiological age
- Potential of surgical procedure
- Patients expectations of recovery
In summary, good surgery needs good physiotherapy. Immobilisation goes against the tide of surgical advances in technology and equipment and early physiotherapy and functional rehabilitation provides focus for achievement, thus promoting recovery.
Kathleen can be contacted via Manchester Shoulder Clinic


