Magnetic resonance imaging (MRI)
With the development of high field NMR scanners and improved surface coil technology, it has become feasible over the last few years to undertake high resolution shoulder MRI. The peripheral location, and unique anatomy of the shoulder joint does pose some technical problems for MRI, however. Surface coils are essential to provide high spatial resolution, and novel coils have been designed specifically for shoulder imaging.[15] Software modifications may also be required (for example, to alter the centre frequency) to allow off-centre zooming.[16] T2-weighted images are essential, but either T-i-weighted or proton density images are also important to assess morphology, and the subdeltoid fat plane. Axial images are obtained, as well as coronal oblique images, in the plane of the supraspinatus tendon, and sagittal oblique images, perpendicular to this plane (Figure 3.11).
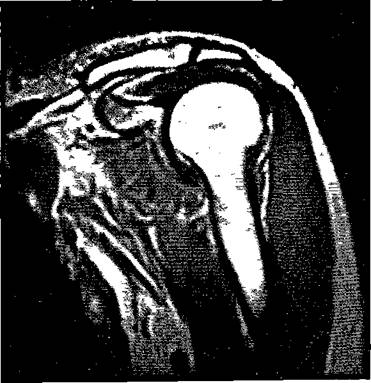
Figure 3.11 Coronal Tyweighted spin-echo image of a normal shoulder showing the long head of biceps, and the rotator cuff lying between the joint and the subdeltoid bursa.
Like ultrasound, there is no clear consensus on the criteria for diagnosis of a tear. T2-weighted spin echo images frequently show areas of high signal within the cuff, but some of these patients will prove to have intact cuffs at surgery. In general, a normal intensity cuff with a normal subdeltoid fat plane is likely to be normal. An area of increased signal in the region of the cuff on T2-weighted images, with normal morphology, and a normal subdeltoid fat plane probably indicates cuff degeneration without a tear. Most patients with a cuff tear show increased cuff signal, or discontinuity. Loss of the subdeltoid fat plane or fluid in the subacromial bursa on T2-weighted images are also very suggestive findings.[17]
In most of the published series, MRI compares favourably with arthrography, although there are always a few tears missed by MRI, but shown by arthrography.[18] Some partial thickness tears are only demonstrated by MRI, however. In impingement syndrome, MRI proved very sensitive to cuff degeneration in one series.[19] However, subacromial injection of steroids can produce MRI changes which mimic cuff pathology. This is a potential drawback, as many patients will have had local injections before being referred for MRI.
Results in recurrent shoulder dislocation are less encouraging, as the normal glenoid labrum is a low intensity structure on most sequences, and is consequently harder to assess. CT arthrography may be more sensitive in the detection of labral pathology, although it can be demonstrated by MRI. Similar reservations also apply to the diagnosis of capsular stripping on MRI. This is readily demonstrated by CT arthrography, as the joint is distended during the procedure. MRI can only detect capsular separation in the presence of a joint effusion.[20]
The accuracy of MRI in the detection of humeral head defects is probably equal to that of CT arthrography.


