Arthroscopic Suture Repair: Morgan technique
In 1959 Viek and Ben[10] described a technique for reattaching the Bankart lesion using pullout sutures. They acknowledged Luckey with the concept. Three 0.3 cm (1/8 inch) Steinmann pins were drilled through the glenoid from the front and then out of the back of the patient, passing through infraspinatus and skin. Pullout sutures were taken through these transglenoid tunnels and tied over on the skin. The sutures were removed at 3 weeks. Morgan and Bodenstab[11] took this concept and performed the operation arthroscopically. The advantages of this technique are its simplicity, the lack of damage to the glenoid neck, and the fact that no metallic hardware is left in the joint.
Method
Set up
The patient is placed in the lateral position and the arm is suspended, using two shoulder holders, in a position of internal rotation.
Diagnostic arthroscopy
This is performed for the same reasons as in the staple repair. Bleeding is controlled by adding 1 ml 1:1000 adrenaline solution to each 31 bag of saline.
Procedure
An anterior portal is made through which a 7mm utility arthroscopic cannula is passed. The Bankart lesion is probed and assessed. The anterior glenoid neck is prepared exactly as for staple repair.
The arthroscopic suture is performed using a specially designed stainless steel suture pin, 2 mm in diameter and 30 cm in length. This pin has a specially sharp pointed tip which is necessary to 'pick up' the labrum. The trailing end of the suture pin has a recessed eye to carry the suture. Two passes of the suture pin are made, the lower one first. The suture pin is introduced through the 7 mm cannula into the front of the joint (Figure 9.12) and the sharp tip is used to spear the IGHL labral complex at their junction. The sharp tip of the pin can now be seen between the labrum and the prepared anterior glenoid rim (Figure 9.13) and the pin is now used to shift the speared soft tissue both superiorly and medially on the glenoid neck in order to tighten up the IGHL labrum complex. The pin is knocked into the prepared bone with a tap from a mallet, in a position about 3 mm medial to the glenoid neck.
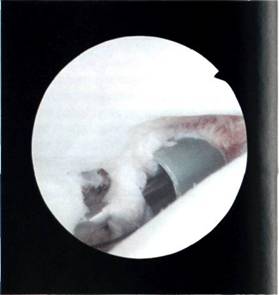
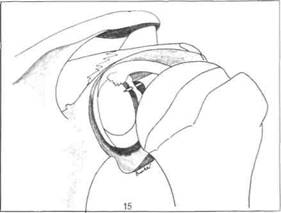
Figure 9.12 The suture pin is inserted through a 7 mm cannula into the front of the joint.
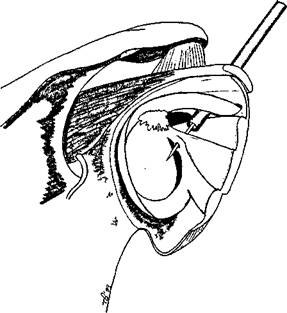
Figure 9.13 The suture pin passes through the labrum.
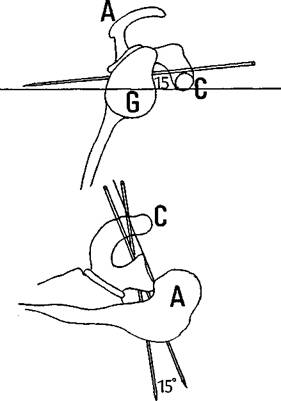
Figure 9.14 The suture pin should pass downward (caudad) 15 degrees, and either parallel to or 15 degrees medial to the glenoid articular surface to avoid damage to the joint surface and the suprascapular nerve.
It is important at this stage to angle the pin for a safe passage through the glenoid. In order to miss the suprascapular nerve on exiting the glenoid, the pin must be angled 15 degrees downward (caudad) to a line drawn perpendicular to the long axis of the glenoid. The pin must also run parallel to the articular surface of the glenoid or, at the most, 15 degrees angled in to the glenoid. Angled any less, the pin may break through into the joint and, angled any more, it might hit the suprascapular nerve (Figure 9.14). Rose has developed a guide, similar to an anterior cruciate ligament (ACL) guide, which can be used to make passage of the pins more accurate. The results are yet to be published.
The pin is then driven through the bone using a power drill and a 5 mm stab incision made over the skin at the point where the skin is tented up by the pin. The pin now passes from the front of the shoulder, through the cannula, the Bankart lesion, the glenoid and out of the back of the shoulder (Figure 9.15). A length of 1 PDS suture is passed through the eye of the suture pin and a haemostat attached to the two ends of the thread. A pair of pliers is now used to grasp the sharp end of the pin and pull it through the shoulder from the back (Figure 9.16) so that it is now replaced by a double thickness length of 1 PDS suture.

Figure 9.15 The pin is drilled through the glenoid.

Figure 9.16 The assistant grasps the suture pin and pulls the suture out through infraspinatus and the skin.
A second passage of the pin is made through the cannula piercing the Bankart lesion about 1.5 cm above (cephalad) to the first passage. The pin is angled parallel to the first passage and drilled through the bone. It is possible to pick up the first suture on the rotating suture pin which makes a mess of tangled suture within the joint. This can be avoided either by being aware of this possibility or by using a reciprocating drill. The second pin should exit the skin about 2 cm above the first pin. Once again a length of 1 PDS is passed through the eye of the pin, and a haemostat attached to the ends. The pliers are then used to bring the second suture through the glenoid.
At this point, there are two doubled threads of 1 PDS coming out of the cannula, each with a haemostat on the end. The two doubled threads are tied together with a double square knot and the excess trimmed off (Figure 9.17). The sutures are cut from the suture pins at the back and replaced with haemostats and by pulling on these haemostats the knotted PDS suture disappears down the cannula and comes to rest on the Bankart lesion. Further tension from behind pulls the Bankart lesion down on the prepared glenoid neck where it will be held until it has healed.
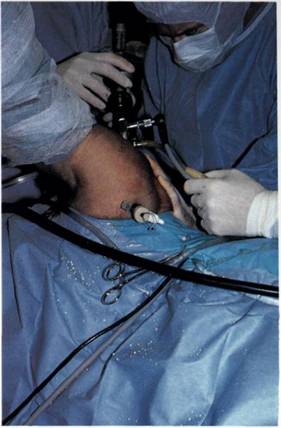
Figure 9.17 The sutures are tied together firmly and the excess cut off.
The only remaining problem is what to do with the suture at the back. A small stab incision is made between the two exiting pairs of sutures and each is retrieved subcutaneously using a haemostat and brought out through the central stab. The two pairs of threads are then tied using a double square knot over the fascia of infraspinatus. A hook probe is then inserted through the cannula and the repair is tested. If all is satisfactory, the cannula and arthroscope are withdrawn and the puncture sites are closed.
Postoperative regime
The shoulder is immobilized in internal rotation for 6 weeks. Approximately 10 days postoperatively, the skin sutures may be removed and the patient is allowed to remove the shoulder immobilizer three times daily for elbow extension exercises. The patient is allowed to shower, as long as the arm is kept in internal rotation. At 4 weeks, active assisted and Codman pendulum exercises are used under the physiotherapist's direction. At 6 weeks, TheraBand exercises are used to strengthen the rotator cuff. Vigorous exercises including contact sports and throwing are not allowed until 6 months after the repair.
Results
Morgan presented his 2-5 years results at the American Academy of Orthopaedic Surgeons' 1989 meeting.12 Of 60 patients, 55 had a Bankart lesion, all had a positive anterior apprehension sign, and none were lax jointed or had a sulcus sign. Follow-up was graded by the Rowe assessment at an average of 37 months. There were only two failures: one redislocated playing American football, fracturing his glenoid neck at the same time, and one subluxed. One patient had a neuropraxia of the medial antebrachial cutaneous nerve, but no evidence of injury to the suprascapular nerve and no problems with the suture over infraspinatus. Of the 96 per cent graded as excellent, which is comparable to the best open series, 53 had excellent results, including 46 who achieved a full range of shoulder movement, and 7 who lacked 5 degrees of movement.


